A team of researchers publishing in the Nature publication Molecular Psychiatry has described how a newly discovered interaction of amyloid beta (Aβ) is being used in the development of a vaccine for Alzheimer’s disease.
A specific antibody for truncated Aβ
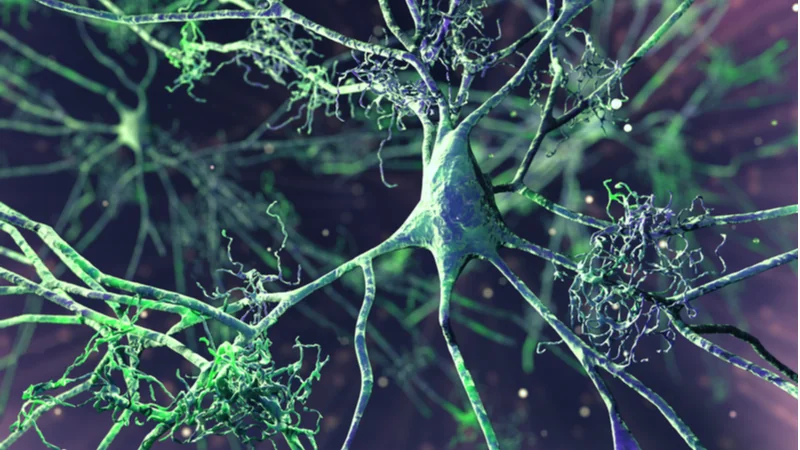
The biochemistry of Alzheimer’s is extremely complicated. Aβ is not always one molecule with a consistent shape; rather, it comes in multiple forms of varying lengths. Targeting the full-length version of Aβ has not proven particularly successful as a clinical strategy, so these researchers have chosen to target the shorter (N-truncated) forms of Aβ.
These shortened variants have been noted as being abundant in the brains of Alzheimer’s patients [1], and their toxic effects have been researched [2]. Previous research had discovered that the antibody NT4X was able to target some of these N-truncated forms [3], and in this paper, the researchers describe how TAP01, a family of antibodies, can be used to target these forms.
A never-before-seen interaction
In this paper, the researchers go extremely deep into the fundamental interactions between a specific form of Aβ and the TAP01 antibody. This “hairpin” formation, which forms when it is bound by TAP01, has never been described in previous research.
The researchers capitalized on their discovery by immunizing a mouse model of Alzheimer’s disease with a cyclic, partial version of Aβ. They found that the mice developed antibodies as a result and that their amyloid plaque levels were closer to those of wild-type mice, which do not develop Alzheimer’s disease. The researchers then injected another group of mice with TAP01_04, a humanized variant of TAP01, and received similar results through this passive immunization.
Significant benefits
Both active and passive immunization were shown to be highly effective in preserving neuron numbers and cognition. Treated mice had roughly twice the number of neurons in the CA1 region of the hippocampus, and their performance on the Morris water maze test was much better than that of their untreated counterparts.
Active immunization was also found to be beneficial in stabilizing blood glucose metabolism. Treated Alzheimer’s mice were slightly better at this than their untreated counterparts, although they were still substantially outperformed in this area by wild-type mice.
Conclusion
First and foremost, it is important to note that this antibody is, and is intended to be, specific to this soluble version of circulating amyloid beta and does not react with the existing tangles present in the brains of Alzheimer’s patients. This has positive ramifications, as the researchers point out: it increases its bioavailability, as the antibody does not get trapped inside tangles, and thus reduces the chance of dose-limiting side effects.
The researchers suggest that both active and passive immunization are potential treatment modalities for Alzheimer’s disease and that both should be explored in human clinical trials. If the passive method is shown to have clinical benefit and passes such trials, it will represent a breakthrough in treating Alzheimer’s; if active immunization is shown to be beneficial for human beings, it will represent an actual vaccine for Alzheimer’s disease.
Literature
[1] Portelius, E., Bogdanovic, N., Gustavsson, M. K., Volkmann, I., Brinkmalm, G., Zetterberg, H., … & Blennow, K. (2010). Mass spectrometric characterization of brain amyloid beta isoform signatures in familial and sporadic Alzheimer’s disease. Acta neuropathologica, 120(2), 185-193.
[2] Bayer, T. A., & Wirths, O. (2014). Focusing the amyloid cascade hypothesis on N-truncated Abeta peptides as drug targets against Alzheimer’s disease. Acta neuropathologica, 127(6), 787-801.
[3] Antonios, G., Borgers, H., Richard, B. C., Brauß, A., Meißner, J., Weggen, S., … & Bayer, T. A. (2015). Alzheimer therapy with an antibody against N-terminal Abeta 4-X and pyroglutamate Abeta 3-X. Scientific reports, 5(1), 1-14.