Using a novel 3D lung organoid model, new research published in Cell Stem Cell has shed light on the body’s infection response to COVID-19.
Read More
Generating lung tissue in vitro
Lung tissue regeneration is an elusive scientific goal that would have a major implications for treating patients in need of lung transplantation. Relative to other organs, lung tissue is particularly difficult to replicate. Its mechanical properties are imperative to its function, as is its architectural structure, both on the micro and macro scales. Furthermore, there are several types of cells found in the lungs that are particularly difficult to grow in vitro. While manufactured lung replacements are far away from the clinic, some small-scale, lung-on-a-chip tissues have been developed.
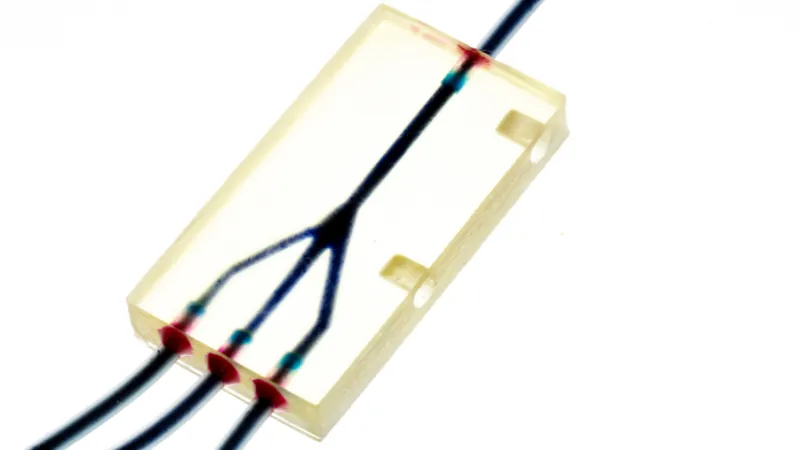
In particular, human alveolar type 2 (hAT2) cells, one of two types of cells that comprise the pulmonary alveoli, do not proliferate and survive in the long term under in vitro culture conditions. However, a team of collaborators between several United Kingdom and Korean institutions was recently able to successfully culture hAT2 cells long-term [1]. After isolation, the cells were suspended in 3D on Matrigel hydrogel and exposed to a specialized composition of growth factors.
Under these conditions, the cells still grew very slowly (approximately 35 days per passage), but they continued to thrive much longer than in any previous studies (up to 8 passages). Their results indicate that the cells continued to proliferate, expressed characteristic proteins for hAT2 cells, and even formed alveolar-like structures. In particular, the Wnt pathway, activated by the supplement CHIR99021, appeared to play an important role in this process.
Studying COVID-19 Infection with hAT2 Cells
However, the researchers were not finished yet. Rather, they used their novel accomplishment to test the effects of COVID-19 infection on their alveolar cells, one of the first cell types typically exposed to the virus in people. The researchers confirmed successful infection of the hAT2 cells and then compared the cells both over time and against uninfected cells.
The cells were characterized in depth using a variety of techniques, including RNAseq analysis and single-cell transcriptome profiling. Viral replication was active within hAT2 cells the first day after infection. COVID-19 infection resulted in dramatic transcriptional changes. The cells were largely homogenous before infection, but they deviated significantly afterwards and became much more heterogeneous. Several of these changes present interesting lines of future research to unpack further. Additionally, single-cell transcriptome profiling was able to detect infected cells more sensitively than other traditional methods, possibly by catching newly infected cells that contained high viral transcripts but not yet high viral protein levels.
In summary, our study highlights the advantages of h3AC models to elucidate the pathogenesis of SARS-CoV-2 infection in alveolar stem cells. Our data will be a great resource for the biomedical community for deeper characterization of viral disease. We believe that our models will enable more accurate and sophisticated analyses in the near future, especially for studying the response to viral infection within vulnerable groups with aged or diseased lungs, providing an opportunity to elucidate individual patient responses to viral infection. Furthermore, our models can be combined with other techniques, such as co-culture experiments with immune cells and in vitro screening of antiviral agents. We believe that our models are also applicable for the study of basic biology and other diseases in hAT2 cells.
Conclusion
This highly impactful and timely research simultaneously makes major contributions to the field of lung regeneration and to our fight against the current global pandemic. Of course, as with all scientific studies, the results should be taken with caution. Models were established using cells from only 14 donors, who may not be representative of the larger global population. Further, these donors had healthy lungs, and we know that the most vulnerable population to COVID-19 is older individuals, especially if they have multiple comorbidities. The authors acknowledge these shortcomings and plan to look at cells from diseased and older patients in the future. Additionally, they plan to incorporate multiple cell types, particularly immune cells, into their model to increase its similarity to natural conditions in vivo.
Literature
[1] Youk, J., Kim, T., Evans, K.V., Jeong, Y., Hur, Y., … & Lee, J-H. (2020). Three-Dimensional Human Alveolar Stem Cell Culture Models Reveal Infection Response to SARS-CoV-2. Cell Stem Cell, Epub ahead of print. doi: 10.1016/j.stem.2020.10.004