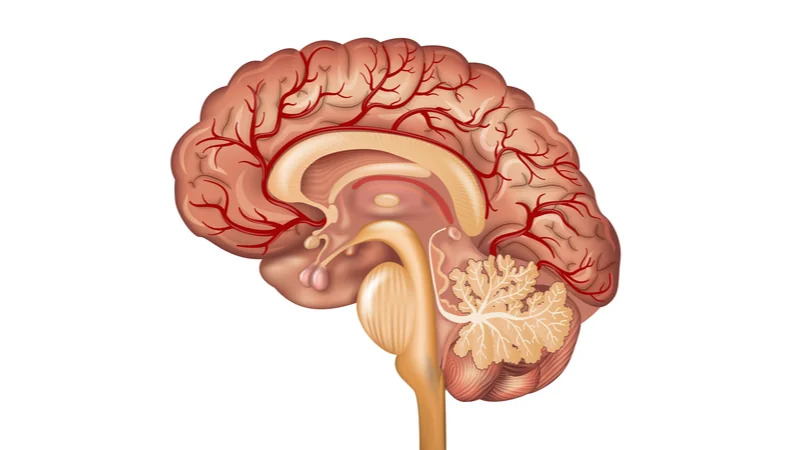
Researchers publishing in Aging have found that enlarged perivascular spaces (ePVS) in the brain are correlated with vascular disorders [1]. These spaces, which are part of the brain’s glymphatic system, allow for the drainage of potentially dangerous metabolites such as beta amyloid [2].
A known biomarker of brain disorders
As they become enlarged, perivascular spaces become visible through MRI imaging. This enlargement represents microvascular damage and brain degeneration [3], and it is associated with increased cognitive impairment and risk of stroke [4]. Prior research has found that the location of ePVS reflects different types of disease: lobal ePVS signify issues with amyloid beta, while deeper ePVS signify hypertension [5].
A large, well-known cohort study
This research builds upon prior work, using the well-known Framingham Heart Study cohort to ascertain the relationships between known risk factors and ePVS. After excluding people for stroke, a total of 3,710 people with 4,101 MRI records became part of the study.
The determination of ePVS was made using rigorous criteria, including placement, size, and signal intensity. Both of the measured brain regions were given grades from I to IV based on ePVS prevalence. The study also measured other well-known biomarkers of vascular health, including blood pressure, BMI, cholesterol, and diabetes.
The researchers then correlated the prevalence of grades 3 and 4 of ePVS with these other biomarkers, and the results were as expected. Systolic and diastolic blood pressures were both correlated with ePVS in lobar and basal regions. Hypertension was very significantly correlated with ePVS in each of the regions, and prehypertension was correlated with basal ePVS. Smoking, age, and the use of hypertensive medication were also significantly correlated with ePVS in both regions.
Interestingly, while there were tendencies, cholesterol, lipids, and diabetes did not have significant effects on ePVS.
Conclusion
This was a relatively simple study with a straightforward conclusion, but that conclusion puts together vascular issues in the body and in the brain. While a causal link has not yet been elucidated, there is clearly a strong correlation between this particular aspect of brain dysfunction and greater cardiovascular issues.
Literature
[1] Lara, F. R., Scruton, A. L., Pinheiro, A., Demissie, S., Parva, P., Charidimou, A., … & Romero, J. R. Aging, prevalence and risk factors of MRI-visible enlarged perivascular spaces. Aging, 14(undefined).
[2] Schley, D., Carare-Nnadi, R., Please, C. P., Perry, V. H., & Weller, R. O. (2006). Mechanisms to explain the reverse perivascular transport of solutes out of the brain. Journal of theoretical biology, 238(4), 962-974.
[3] Gouveia-Freitas, K., & Bastos-Leite, A. J. (2021). Perivascular spaces and brain waste clearance systems: relevance for neurodegenerative and cerebrovascular pathology. Neuroradiology, 63(10), 1581-1597.
[4] Francis, F., Ballerini, L., & Wardlaw, J. M. (2019). Perivascular spaces and their associations with risk factors, clinical disorders and neuroimaging features: a systematic review and meta-analysis. International Journal of Stroke, 14(4), 359-371.
[5] Wardlaw, J. M., Benveniste, H., Nedergaard, M., Zlokovic, B. V., Mestre, H., Lee, H., … & Black, S. E. (2020). Perivascular spaces in the brain: anatomy, physiology and pathology. Nature Reviews Neurology, 16(3), 137-153.