Emma Teeling is a professor at University College of Dublin, and her research focuses on bats. In this interview, Emma explains why many bats, despite having tiny body sizes and leading very metabolically demanding lifestyles, are so amazingly long-lived. Will we ever be able to learn these animals’ secrets of beating the odds? Emma is optimistic on that.
How did you get into science in general and geroscience in particular?
I did an undergraduate in zoology in University College Dublin in Ireland. I was very interested in trying to understand different processes that would allow species to evolve. I originally was a field biologist and did my master’s degree in animal behavior, but I realized that to understand real evolution and all the different evolutionary histories and environmental changes that led us to have the species that inhabit our planet, I had to embrace genetics.
I decided I’m going to study genetics, but I wanted to study mate-choice behavior in domestic cats. After I got my Master’s, I took a year out, I traveled around Africa, and then I started writing applications to various universities – that it would be a great idea to do a PhD on mate-choice behavior in domestic cats.
I was very happy with this new project idea, but I was looking for somebody who had money to fund it. I saw an advertisement to apply for PhD up in Queens University at Belfast to look at the evolution of echolocation in bats, to try and make evolutionary trees by using genes.
Way back in the “Dark Ages”, when I started my PhD, it took seven years to sequence 400 base pairs of a spider silk gene, so this was a brand new exciting field of biology. However, I thought: OK, but this man has money, so I approached him with my project – why don’t we spend your money on my project?
So, you pitched your cat idea to him?
I did. I went to Belfast, pitched the cat idea, but they said to me: “Why are you interested in these cats? Looks like you’re more interested in genetics and evolution. Why don’t you apply for this position to study bats?” And so I did, still hoping I could get that cat project funded. Long story short, I got a full scholarship in Belfast to study echolocation in bats by building phylogenetic trees from genes. Within six weeks of starting this project and reading more in depth about bats, I was completely hooked. They are the most fascinating of all mammals. So, I started to study bats by chance.
First, we found that our understanding of how bats evolved was completely wrong, including our understanding of how echolocation evolved. For instance, we found that echolocation either had multiple origins or was lost in the big fruit bats. I was very lucky because we were using new cutting-edge molecular technology, revolutionizing and rewriting the mammalian tree of life. The whole field was moving in this direction – we could now sequence genes, make evolutionary trees, understand how traits evolved.
The next thing was to realize that bats do some really unusual things. They live for a ridiculously long time despite their small body size, without showing signs of aging. They tolerate many viruses without getting sick.
I started to read literature about bat lifespan. There’s a pattern in nature that big things live slow and long, while small things live fast and die young. Bats are some of the smallest mammals on earth, but most have very long lifespans for their body sizes.
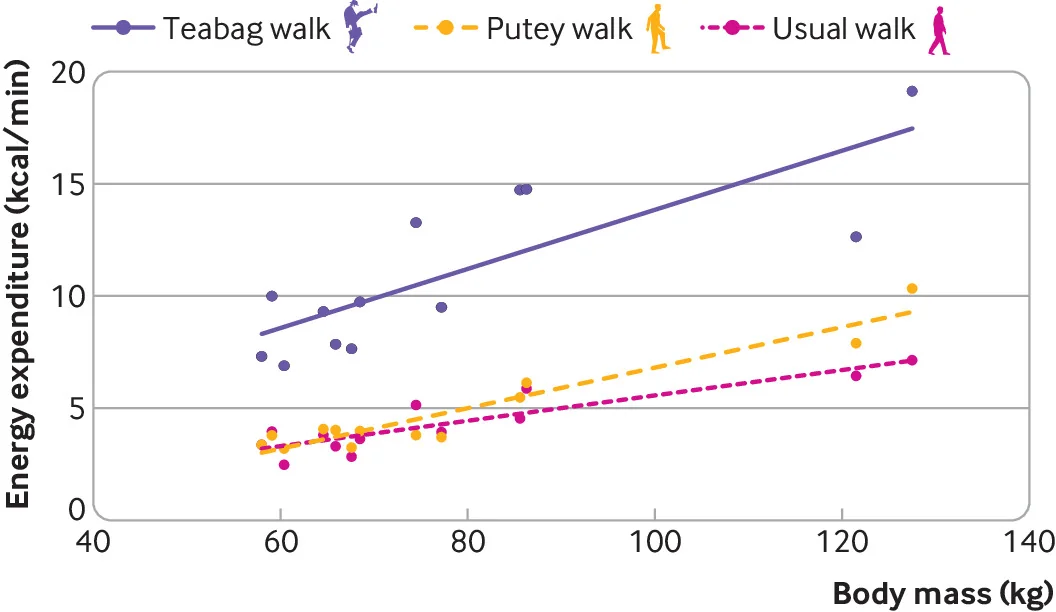
Now, flight is the most metabolically costly form of locomotion. Bats use up to three times more energy than any other mammal of the same size. Having a very high metabolic rate typically can be very damaging. Cells produce a lot of reactive oxygen species that break up DNA, stimulate the immune system, and generally wreak havoc. Arguably, this is what drives aging. It looks like bats have evolved something to deal with these deleterious effects of flight.
Another thing I was very interested in is what bats do to avoid cancer. They really have the lowest cancer rate of all. They also tolerate all those viruses without getting sick. Why are there so many different types of viruses in these bats? These questions were formed in 2001, before we had this horrible pandemic right in our face.
Three years later, I was able to return to Ireland, got a position in UCD (University College Dublin), something I’d always dreamed of. I managed to get some nice grants to study bumblebee bats in Thailand, I got a presidential young researcher’s award. But what really changed my relationship with aging research was the grant I was able to secure from the European Research Council.
I had a second baby, struggling through all of this. Believe me, life can be hard for an academic mother trying to push science in Ireland. We teach an awful lot. But it was always in the back of my mind: we need to understand how bats do not get cancer. I’ve always said that the key to understanding how we can survive cancer lies in bats.
The European Research Council is one of the most amazing funding bodies in the world. It funds high-risk, high-gain projects. Anybody can apply, but it’s exceedingly competitive, and when you write this grant, you have to imagine what would you do if there were no barriers. I said I wanted to study bats and understand how they can help us slow down aging. How are their slow pace of aging and their unique immune responses connected, and how is it driven by flight?
There are 19 species of mammals that live longer than humans when adjusted for body size, and 18 of those are bats. It’s as if humans lived to about 250 with no signs of aging. But if you want to study bats in aging context, the longest-lived bats, those of the genus Myotis, there is a problem: they don’t do well in captivity.
One of my PhD students had worked in France, and the French care about their wildlife. And there was this grassroots organization called Bretange Vivante. It’s a conservation organization that had been studying this colony of long-lived Myotis bats for about 20 years.
They caught the entire colony in 2010. These were very long-lived bats that were also large enough for us to non-lethally sample them. They were caught and tagged as babies, and then we would recatch them. So, when I started writing the ERC grant, I was very lucky to find this population of long-lived Myotis myotis, or greater mouse-eared bats, in Brittany. It came to an integrative collaboration with this grassroots organization that was interested in ecology, because bats are so important for the ecosystem to function.
The only way you can measure a bat’s age is you catch it as a baby, say, in 2010, you put in a little microchip, like you would in a dog or a cat, and then, when you catch the same individual in 2020, you know it’s 10 years of age. What was really cool about this population is that they were captured every single year by this organization, and they were big enough so that we could take non-lethal samples.
If you want to study an animal in the context of aging, you have to be able to sample it every year as it ages, which means you have to recapture it. What happens with these species is that the females come back to the same roost – in this case, beautiful old Gothic churches. Like me, they give birth in the same place they were born in!
I wanted to be able to take a wing puncture and less than 140 microliters of blood. So, the idea was to take these samples, and look at biomarkers of aging. We wanted to compare young, middle-aged, and older bats and see whether they show the same pace of dysregulation with age as humans do, and what are the mechanisms that regulate this?
We wanted to look at telomeres – do they shorten in bats with age or not? We also wanted to look at their mitochondria – with such a high metabolic rate, do their mitochondria show the level of oxidative damage that would be expected given all the free radicals that are produced? We wanted to sequence the entire blood transcriptome, because blood is an overall proxy for health in multiple tissues. We were also going to look at their microRNA that can potentially regulate many different levels of transcription, at the genomes, at DNA repair mechanisms, at their immune system to see any evidence of adaptive selection going on.
With this, I got the grant. I couldn’t believe my luck. It’s one thing to write all this down on paper and to convince reviewers, but the first year, oh my goodness gracious, it was difficult. However, you have to make it work, and nobody has ever done anything like this before, because it’s bloody well hard.
My Irish group had very bad French, and people from that organization in France had no English. It was a clash of cultures, but we all had to work together, because we have three weeks in the entire year to sample this colony of over 500 individuals. The entire village would come together and help us put up traps in these churches. So, we capture the bats, measure them, weigh them, microchip the babies and flash-freeze the samples.
We had to work out how to do it, and it was so hard. I remember lying in the grass at three in the morning and crying, going: “What on earth have you done, you stupid woman?” But in the end, we made it work.
Yes, it is pretty amazing. I was wondering, considering these animals are so tiny, does taking even non-lethal samples affect their fitness in any way?
It does not. We were obviously worried about it, so we did population predictions to see if there’s a change in terms of animals returning year after year. If taking samples affects fitness, the manipulated bats would die in greater numbers, but that didn’t happen. Also, we catch the same females year after year, and they are all pregnant. So, it looks like our manipulation doesn’t affect them, otherwise we wouldn’t be doing it, because they are protected species.
If bats barely age, what do they die of?
First, bad weather. A very wet spring is hugely problematic for bats. Typically, the recruitment back after year one is about 55%, which means you lose half the babies every year. But once they get to two, you don’t seem to lose them. What correlates with fitness, for instance, when we look at telomeres, is weather, not aging. Think about their biology. They have their babies in July, then they start hibernating in October, and they have to get really fat in August and September to be able to survive hibernation.
Their first year, they have to be born early enough to be able to get fat enough to survive the winter. So, what these females can do if spring is really bad when they wake up from hibernation, and they’re pregnant because they’ve made it in the swarming, is they will slow down their gestation to match it with the food supply. The babies are born later and have less time to get fat. We have found a correlation between stress and telomere dynamics, and it’s been confirmed in many different populations of bats. So, bad weather is a major threat. And they also get eaten by owls.
So, what you’re saying is that stress affects fitness that affects telomere growth?
Yes. Let’s not forget that as the longest-lived bats age, bats of the genus Myotis, their telomeres don’t shorten. On the cohort level, you see this change that can only be attributed to bad environmental conditions. In the US, bats also die of white-nose syndrome, which is a fungal disease of the skin. It grows when the bats are in hibernation. When they drop down their temperature to nearly four degrees, you find fungus growing. So, these are the things bats can die of.
Interesting. In naked mole rats, when we put them in sterile lab conditions, we can’t really tell what their true maximum lifespan is because they just refuse to die, at least the queens. I understand bats don’t like captivity, but theoretically, if we could put them in a sterile environment that were to their liking, what do you think their maximum lifespan would be?
It’s a great question, but I actually don’t know the answer. Obviously, I don’t think they’re immortal. Yes, we haven’t optimized our husbandry yet, but say, if we were to make a perfect environment for these bats, would they show signs of senescence? I honestly don’t know.
Let’s talk about some concrete anti-aging defenses they have. So, they don’t experience telomere attrition – or, as I understand, they regrow their telomeres during hibernation?
All of this is not published yet, so for the record I can only say that potentially, they could be doing it in hibernation. A better question is, how are they maintaining their telomeres? In cell lines, when we looked at RNA, we didn’t find any evidence for telomerase expression, but maybe if we look at the protein level, we will see something. It looks like bats are maintaining their telomeres, either via telomerase or an alternative mechanism. Either way, they are doing this without getting cancer. The big question is, how do they not get cancer?
We looked at the whole blood transcriptome in young, middle-aged, and older Myotis bats to see if there were any age-related patterns. When you look at how the blood transcriptome changes in bats, you see a huge difference between babies and one-year-olds – that’s because they’re developing. After that, there’s very little change. In mice, for example, there’s a huge difference.
You also find that as they age, they have this immune balance, like human supercentenarians. They have high inflammation, but also high anti-inflammation to keep the homeostasis. There’s also evidence of maintaining mitochondria.
The big difference is their ability to repair DNA that goes up with age. They maintain a very tight cellular regulation system. I think they’re really good at regulating cell division. Potentially – this is just me thinking out loud, there’s not a lot of evidence for it, but this is what we have to do to move the field forward – potentially, they have a much better immune regulation of cells that go malignant.
We need to ask the question, what are they doing to prevent cancer? They somehow manage to maintain long telomeres without the side effect of getting cancer. We’re looking into that at the moment.
This is where the immune system comes in. We talked about inflammation. As we age, we become highly inflamed, which is now considered as a major driver of aging and disease. Bats have a way of getting that balance right, and this potentially evolved from flight.
Flight is highly metabolically costly and drives inflammation. Bats are the only mammalian order that has achieved true self-powered flight and therefore must have evolved mechanisms to control the constant sterile inflammation they experience from flight.
Interestingly, bats are missing these things called PHYIN genes, the entire family. PHYIN genes make proteins that make an inflammasome which is usually required for the immune system to fight disease by causing inflammation. However, an out-of-control inflammatory response and too much inflammation causes problems. Bats have lost these key genes. The only mammalian order to do this. This means they have this modulated immune response that’s very different from what we see in most other animals.
What you find when you sequence bat genomes is that bats have this expansion of anti-viral genes. They’ve lost these inflammatory genes, they have selection on downstream immune system genes, and they seem to have evolved this perfect Goldilocks response – enough inflammation to control the virus and then enough anti-inflammation to control their immune response.
Because viruses are abundant in their colonies?
The question is, which came first? I think they first had to evolve this anti-inflammatory response to be able to deal with the high levels of inflammation that they experience from all their ROS. They’ve had to evolve this dampened immune response to DNA damage and to ROS damage induced by flight.
Potentially, they lost their PHYIN genes to cope with this, but then they had to evolve a different mechanism to deal with all the pathogens. I think this is how evolution acts: one thing gets broken, one thing gets fixed, or maybe it happens altogether.
My hypothesis is they had to evolve this very aggressive anti-viral response dampened by an equally aggressive anti-inflammatory response, and the two go hand in hand. This means, when they get sick from a virus, they are able to first neutralize the virus, and then neutralize their own immune response.
So, they don’t get cytokine storms?
Exactly. There’s been research recently when they infected live bats and also bat cells with SARS-CoV-2, and the bats didn’t get sick from it. The question is how? There’s a theory about aging that inflammation is really at the heart of it all. Every one of the pillars of aging can be driven by inflammation, and the immune system plays a huge role.
I think bats have done more than just that. I don’t know if you’ve heard of this hypothesis by Claudia Franceschi called “garb-aging”. The idea is that aging is driven by accumulation of damage. Damaged DNA, damaged proteins, not being able to remove them.
The idea is that bats had to evolve mechanisms to limit, repair, and remove damage. They do this by limiting their inflammation. They also have brilliant DNA repair mechanisms. But there’s another thing bats do – as they age, their ability to remove damage via autophagy increases. It decreases in us, humans, and also in mice, but it increases in bats. We saw that in our field and lab studies.
Interestingly, autophagy is also viral regulation. Again, there’s this link between repairing damage and removing damage but also being able to deal with pathogens. I think the two things have to go hand in hand.
This sounds like a case of “what doesn’t kill me makes me stronger”, meaning that bats had to evolve those coping mechanisms that ultimately make them live longer.
Yes, I think that long life is a side effect of evolving protective mechanisms to deal with flight. Being able to carry all those viruses is also a side effect of those mechanisms that protect them from the pathogenic effects of flight.
Here’s another hypothesis that’s quite provocative. When you look at bats’ genomes, they have the smallest genome size of all animals, yet they have the highest diversity of integration of viruses within their genome.
So, a small genome is harboring all those integrated viruses. Why would you do that? Why would evolution allow for this? Potentially, this allows for more genomic plasticity, for evolution, for change, but maybe this is selected for in bats.
We have a paper that was just accepted in Cell, a collaboration with Professor Thomas Zwaka in Mount Sinai hospital in New York. He was very interested, when the pandemic broke out, to study bat lung cells to understand what mechanisms bats have evolved to protect themselves against SARS-CoV-2. The idea was to make induced pluripotent stem cells, but the traditional Yamanaka factors that work in all other animals, didn’t work.
When they tweaked the recipe enough to make those iPSCs, this re-awakened all the endogenized viruses, a plethora of different viruses, and that gives you a huge insight into what viruses bats have survived in the past. Indeed, these fossilized viruses in bat genomes tell a story of a long-evolutionary history of bats and viruses.
When you look at those iPSCs, it looks like a pro-viral environment. We’ve argued in the paper, and it’s Thomas’ hypothesis, that, potentially, it’s adaptive to bats. Maybe this is how they inoculate themselves. It’s just a theory, of course, lots still to do! To understand what’s happening in bats, we need to bring all fields together, we need great minds.
We were able to confirm this in a bat of a different sub-order, and we now can make bat cells in the lab, including all immune cells. We can even make organoids, and this can give us some amazing insights. I firmly believe that the key to extending human healthspan is out there, that nature has already found all the solutions. They are in bats, and we just need to uncover them.
I totally subscribe to this idea that the solution is out there, but even theoretically, how can we benefit from all those mechanisms that have evolved in other species, and how far away are we from doing this?
We’re finding all those things that are happening in bats, but in order to make it work in humans, first you need to put it into a system that humans already know can be compared to their own biology. So, we need to identify the regulators of longer healthspan in bats and knock them into a model system such as C. elegans and see if they extend healthspan.
You can totally do it, and we are currently working on a collaboration with Björn Schumacher. The idea is that once we identify these regulators, which are mostly conserved across species, and if we find out if they have lifespan or healthspan effects on C. elegans, we can then validate it in genetically modified “bat-mice”. Linfa Wang’s group in Singapore has already done this; they’ve shown they can knock bat immune genes into mice and are investigating if they have a healthspan effect.
So, the tools are actually there. But after we have a bunch of targets, which should take us about six years, how do we find the drugs that can help us? As you know, in the longevity field, we have Alex’s (Zhavoronkov) work that can potentially speed this up using AI. You can drug the pathways, but you first have to identify them, that why we need the bats. Luckily, we share the same genes, bats are mammals too.
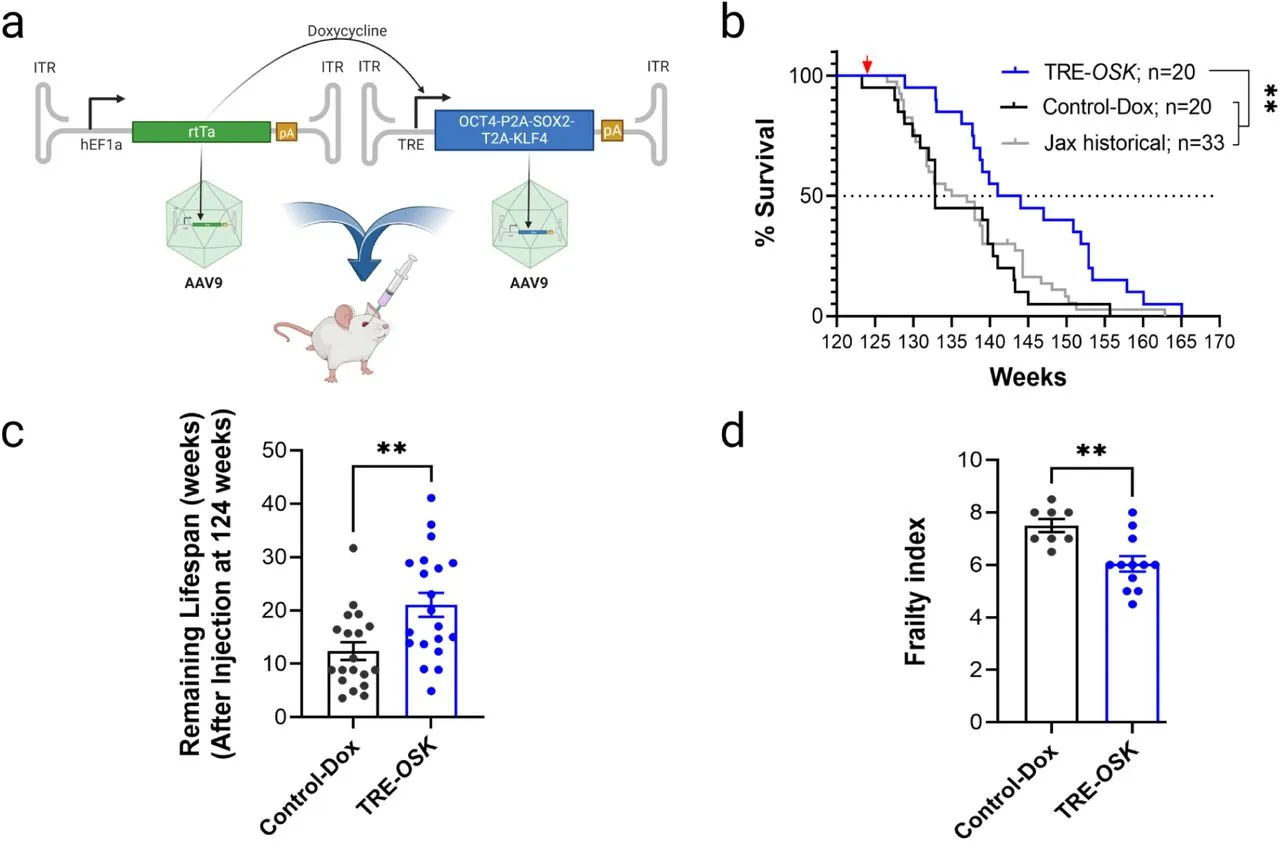
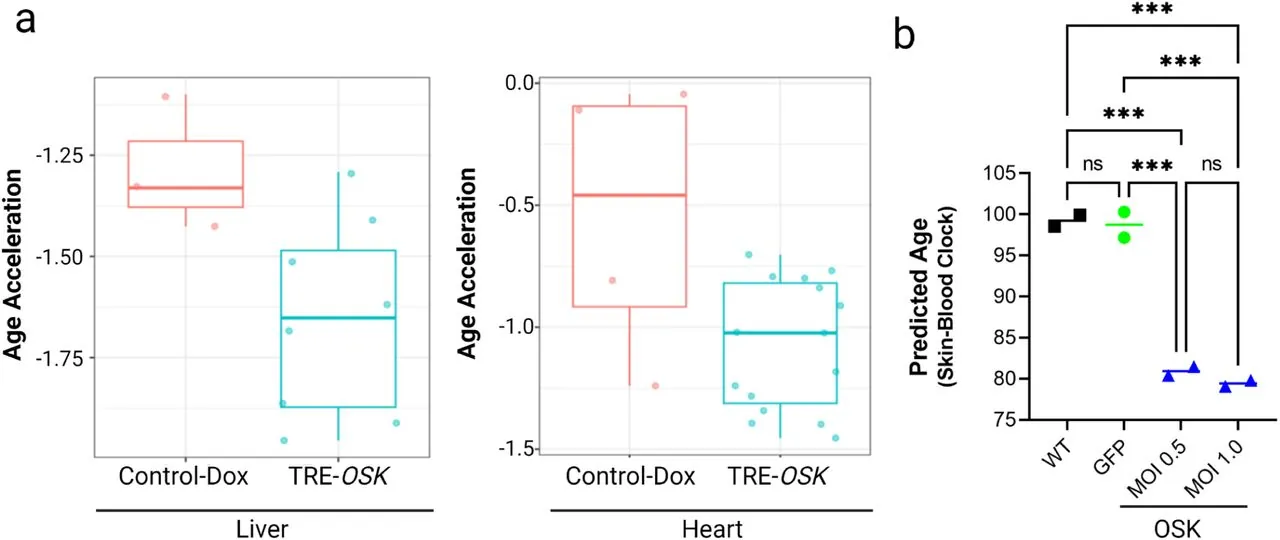
There seem to be two competing approaches, with some geroscientists betting on drugs, and others on less traditional things like gene engineering and cellular reprogramming.
I think it’s easier to take a drug.
The question is whether it’s going to work.
This is always the question, but drugs work, just look at aspirin. I think it doesn’t have to be one or the other, but my problem with gene engineering is, when do you do it? Do you do it at the embryonic stage, at the egg stage?
For me, the easiest thing with bats will be to emulate their immune response, to find out how we can regulate and stop this pathogenic and inflammatory response that you get from diseases and that ultimately kills you.
When the first patients died of COVID-19 in Ireland, I was devastated because my research was ten years behind. We just showed that bats have a certain inflammatory/anti-inflammatory ratio, they have more IL-10 than TNF as disease continues. The doctors in our hospital were using that proxy to figure out whether or not a patient was going to need to go on a ventilator. If they had a bat-like immune profile, where there’s more IL-10 than Il-6 (similar to inflammatory TNF), they weren’t going on the ventilator. This is something you can potentially change with a drug.
Or take DNA repair mechanisms. What do bats do to repair their DNA? They may have an increased level of expression of some central genes as they age. We now have about 20 genes with expression varying wildly in bats and other mammals. They might not be the main effector that would be targeted in humans, but they are in the pathway, and those are pathways that we know how to drug. I think in the near future, our ability to drug pathways will advance.
What’s hampered aging research in the past? Too much focus on short-lived organisms, but there was no other option. We didn’t have the tools to study long-lived species, but we have them now. I think it all has to go together. Fields have to interact with each other and to respect each other, and that’s how we find novel solutions.
Let’s say, worst comes to worst, and we find that it’s not translatable. No matter what, we’ve found a huge, wonderful insight into how the aging process works. We have uncovered brand new biology. Personally, I believe we can solve it, we can apply it to humans, but we need to find the right direction first.
Private capital is playing an increasingly big role in longevity research. Do you think research of long-lived species can be commercialized? Do you have a pitch for a potential investor?
I do. “Every single penny you spend on aging research today could be better placed, because you’ve been studying short-lived organisms who are great at dying, instead of studying animals who naturally evolved longer healthspans and are great at living. We can do this now and I can show you the way”.
We would like to ask you a small favor. We are a non-profit foundation, and unlike some other organizations, we have no shareholders and no products to sell you. All our news and educational content is free for everyone to read, but it does mean that we rely on the help of people like you. Every contribution, no matter if it’s big or small, supports independent journalism and sustains our future.