Six years ago, Dr. Eric Verdin, already a highly acclaimed veteran geroscientist, was catapulted to the forefront of the field when he agreed to lead the Buck Institute for Research on Aging (or simply “the Buck”), a renowned research institution based in Novato, CA. We talked to Dr. Verdin about his vision for the Buck and for the longevity field in general along with his own research, which focuses on several aspects of nutrition, such as the ketogenic diet.
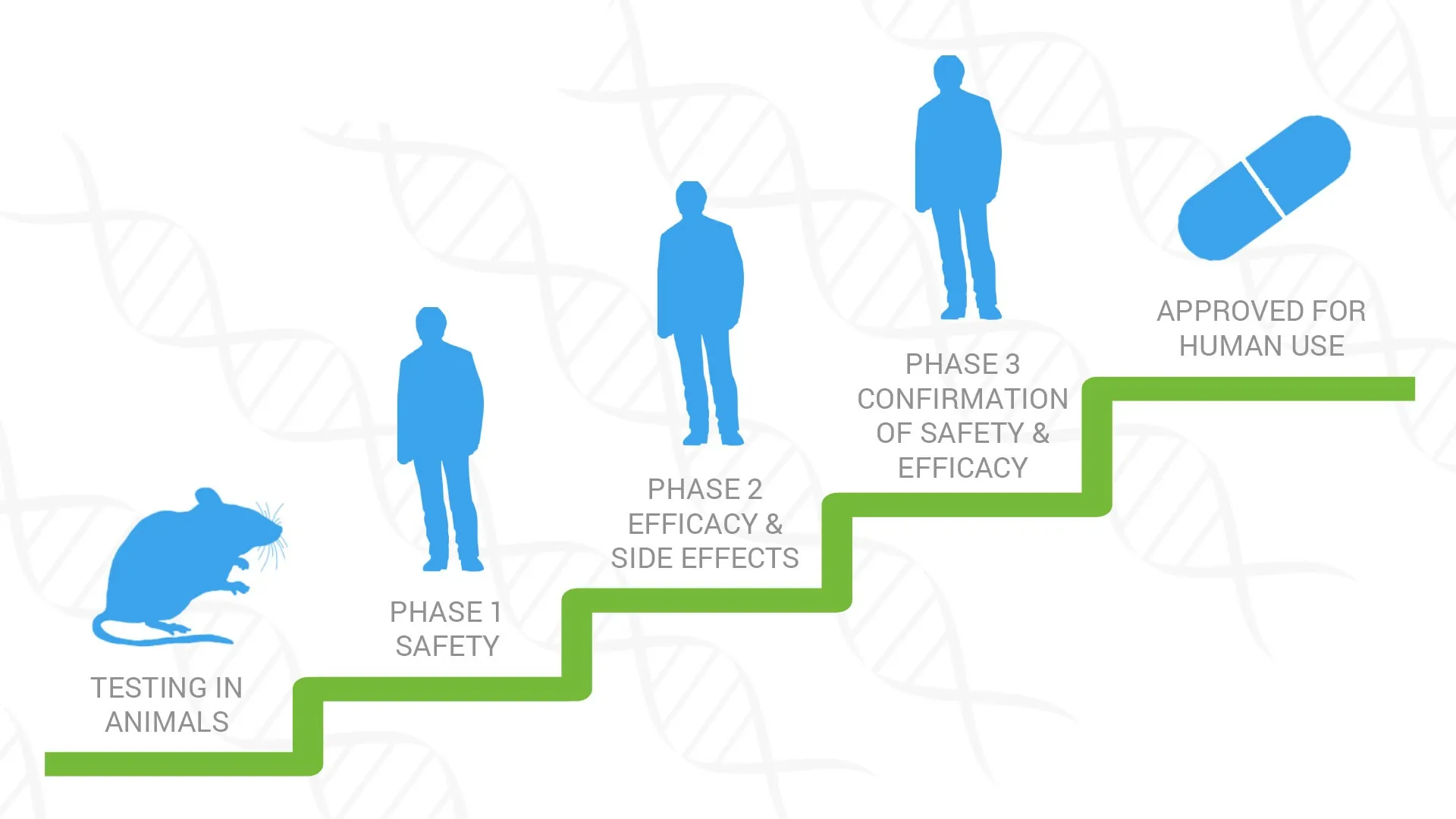
After this interview was completed, we received news about the start of BIKE (Buck Institute Ketone Ester) pilot study, the institute’s first human clinical trial. Dr. Verdin calls BIKE “a hallmark of our growth and the maturation of the field of aging research”, and we will be following it closely.
What was your road to leading the Buck?
I have an MD degree from Belgium. I came to the US right after medical school to do research. I started in Boston, and then I had a whole career across different institutions in the US. My lab initially focused on epigenetic regulation. We ended up cloning a family of proteins called HDACs, histone deacetylases. At that time, my work was primarily on HIV and its epigenetic regulation, but then epigenetics became important in terms of aging.
Back in the late 90s, the field of HIV molecular biology became more saturated, and I was looking for a new field of research. That was the time when all those exciting papers came out showing that aging was a molecular process that you could study using molecular tools.
So, we started shifting to studying epigenetic regulation of aging. In particular, we focused on sirtuins and HDACs. Over the next 15 years, I built my lab doing research on epigenetic regulation of aging. At that time, I was approached by the Buck for the opportunity to lead it. One of the things that led to my selection, I think, was that because of my MD background, I’ve always done basic research with an eye on translation.
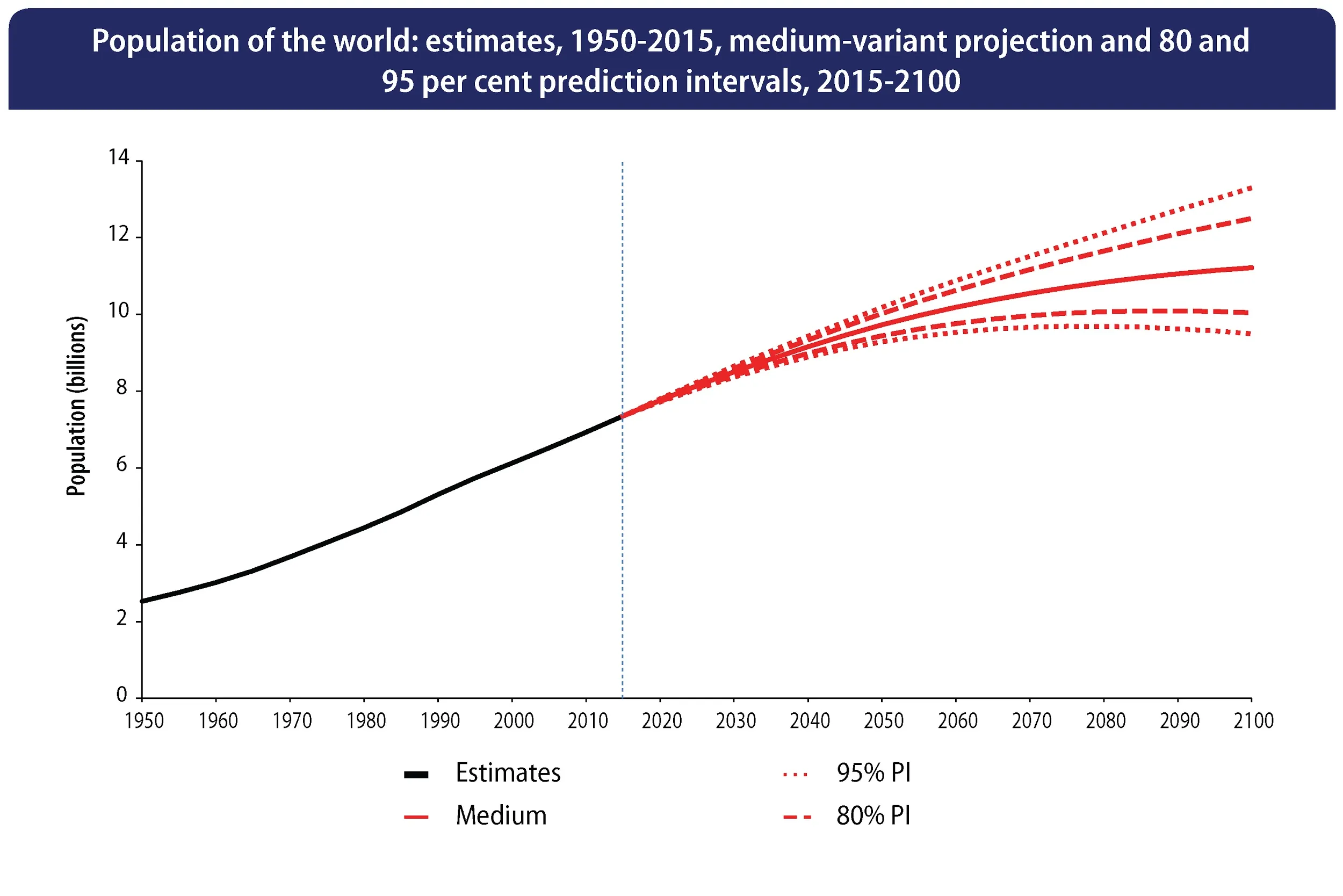
After having been in the aging field for almost 20 years, I started to realize that the field was moving into the next phase, beyond C. elegans and the fly (which, by the way, are amazing models, and we still use them). Geroscientists were beginning to ask some hard questions, like how can all this be translated into humans?
That was the vision that I presented to the board of trustees here at the Buck, and this led them to ask me to lead it. This was a scary transition for me, because I’d never run anything bigger than my lab. To take over an organization of 300 people, a veteran organization in the field, was a bit humbling.
But I was also very excited by this opportunity. I started in late 2016, and it’s been amazing because the field is indeed moving in the direction that the board recruited me to align the Buck with. We are building on basic research, and we still need a lot of it, but we also started building and testing the tools and the infrastructure for clinical trials and doing more human-relevant research.
Were you afraid that you would become mostly an administrator?
I didn’t even know if I was going to like the job, but the short answer is, I love it. First, because I still run a lab and have a very active research program, but I also learned that I love playing a bigger role, being sort of a voice that helps not only the small effort of my own lab but the whole field.
When you run your own lab, it inevitably resembles a cult of personality – it’s “the Verdin lab”, right? This is how people think about it. A lot of it is around yourself, and I’ve always felt that at some point in your life, you have to be able to look beyond yourself and to give to either a field or an organization.
It’s not been easy to learn, and I had great guidance from my board and from other people who helped me, who were there before. Now, five years later, I feel comfortable in this new role, and I relish all the different aspects. In some way, it’s the best job in the world because I can still do research, but I also can influence the whole field that I think is going to have a massive impact on healthcare and human health in general.
You were sort of forced into the role of an advocate for the field, and I know that you have contacts with decision makers, politicians, and so on. Do you feel a change in their attitudes? Is the tide turning?
Yes, the tide is definitely turning, and we see this in the amount of interest that our field is generating. 20 years ago, aging was a field of research that serious people would warn you not to go into. This has completely changed due to the incredible work of establishing the science and demonstrating that aging is a tractable biological problem that we can not only study but also modify. So, the visibility of the field is a reflection of everyone’s effort.
The biotech world, I think, has fully embraced aging. This includes big players like Altos and Calico that enter the field, creating a lot of excitement.
The second element is donors. Here in the Bay Area, we have a whole ecosystem. Our field has been colored by the fact that a lot of tech billionaires have given money, but they are not the only ones. We’re getting money from everybody, which is a good sign that the field is being recognized as a serious one.
There are two more constituencies that we must address where we haven’t made as much progress. One is the medical world, and the other is the political world. They both will be critical in facilitating this transition.
Why has it been slower? First, politicians tend to come last in terms of being aware of what’s happening, but I can point at several efforts that are taking place, such as the Alliance for Longevity Initiatives. I’ve been in touch with several such groups that share the same goal: to reach out to politicians and make them aware of the potential of this field.
Finally, there’s medicine itself. We’re not going to make this revolution without the medical world. Initially, the approach was “we’re going to replace medicine”. It’s not a constructive way, because if you’re a physician, and somebody comes and tells you, “We’re going to replace you, we know better”, your first reaction would be to fight this.
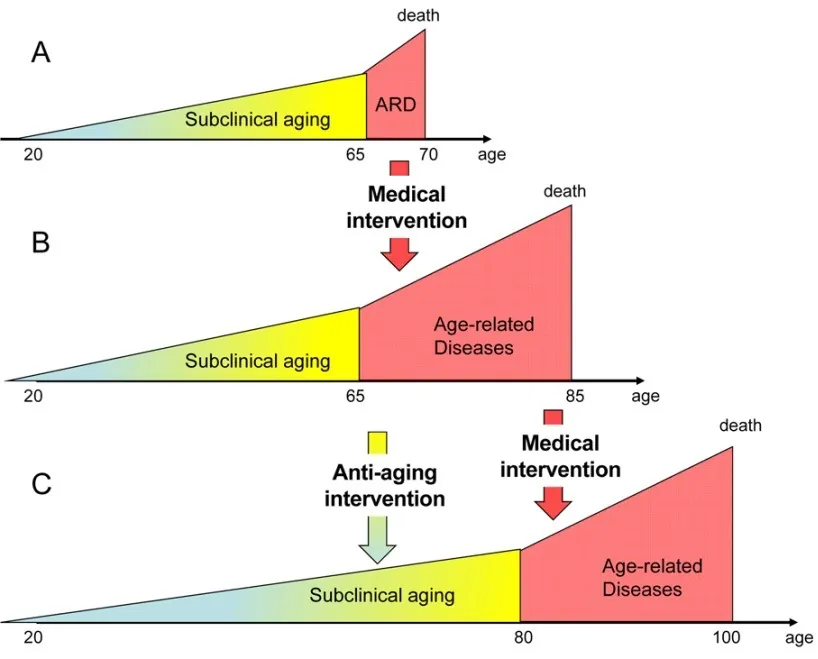
So, I’ve changed my thinking about it. I think the science of aging is not going to replace medicine, but instead it will add an important new dimension. What medicine is doing very well is to cure disease. If you have cancer or a heart attack today, you’re not going to see a geroscientist. We wouldn’t be able to help you.
What we are bringing to the table is this idea of preventing these diseases from occurring in the first place. We can make medicine much more preventative. Based on the premise that aging is a lifelong process, the earlier you start treating it, the likelier you will be to prolong your lifespan and prevent the development of disease.
I’m sure you’ve heard about the so-called “geroscience hypothesis” that emerged from the Buck before my time: that aging is the biggest risk factor for all the chronic diseases of aging and that if you slow down the rate of aging, you will be preventing the development of these diseases.
When I describe this concept to physicians, they’re completely on board, but they ask what we can show them. And we do have some early examples with metformin, rapamycin, and so on, but there’s also the whole idea of lifestyle interventions. What can you do today even without a drug to maximize your chances to age well?
This hypothesis became transformative because it was embraced by the NIH. They helped to create the Translational Geroscience Network which is in some way reflective of what we are trying to do. In NIH, you have individual institutes – for heart disease, for lung disease, for immunological disease – and all of them are studying diseases as if they were independent, whereas we know aging to be the biggest risk factor.
Felipe Sierra, who is now the CSO for Hevolution, was the one who brought the Translational Geroscience Network to the NIH, forced all those institutes to work together, and made them realize that we all should be related to aging.
Let’s talk about your research. I think one of the most interesting things that you study is the link between nutrition and inflammation. There is a growing understanding that we’ve probably been underestimating the role of inflammation in aging. Where do you stand on that?
As a scientist, I think it’s a field that has been underappreciated, and it’s lived in its own world. One of the reasons is that immunology is a highly complicated form of biology. And I’m not saying that because I’m an immunologist.
Why is it important in aging, and why it has been somewhat ignored? Some people have worked on the concept of inflammaging – this idea that we develop chronic inflammation as we age. It has been advanced for several years, but it’s shocking that inflammation was not one of the original hallmarks of aging.
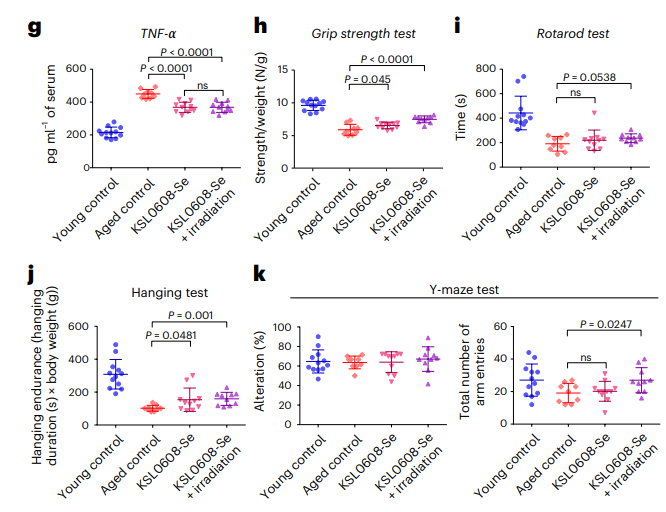
Recent research shows that if you induce aging in the immune system, you can induce secondary aging in all organs. I think it’s a very important finding. We also know that the immune system shows some aging at an earlier point than other organs – take, for example, the thymic involution. The fact that your thymus disappears before you’re 50 has enormous implications on your ability to maintain a proper immune response.
Sadly, many people in the immunology field do not or did not study aging. As an immunologist going to aging meetings, I was always struck by the fact that most people in the aging field knew nothing about immunology and immunologists were not interested in aging. I don’t want to diminish the work of people who are working to combine those two fields, but I see a real opportunity to do a lot more work in this area, and this is what we do.
What about the concept of “anti-inflammatory diet”? How possible and effective it is to decrease inflammation with diet?
That’s a good question. It’s one of those subjects where there’s a lot more information in the lay press than in the scientific world. Currently, I think, the whole concept of pro-inflammatory or anti-inflammatory diets rather belongs to the realm of health podcasts than it is being studied hardcore in the laboratory. Yes, there are some foods, such as those high in saturated fats, that are pro-inflammatory. But when I’m reading articles about this or that anti-inflammatory diet, my question is always, what’s the evidence for this? And when you start looking into it, it’s not that much.
So, a part of me thinks that we should go back and study this. There is certainly a role for inflammation in aging, but the relationship between food and inflammation is not as clear as some people would like to think. For instance, there’s a whole literature that says colored fruits are anti-inflammatory. But what’s the evidence for this? I’m a bit skeptical there.
Of course, the diets that are promoted as anti-inflammatory are healthy, but whether they work solely by lowering inflammation, is much less clear.
But you do think this is something worth exploring, right?
Absolutely, and one thing that’s clear is that inflammation is a central driver of many chronic diseases of aging. The question we don’t have a clear answer to is, why do we develop chronic inflammation as we age? Senescent cells are, of course, one of the mechanisms, as are DNA damage, the accumulation of denatured protein, leaky gut, where your intestinal membrane becomes more permeable, which allows bacterial products to transduce into the bloodstream. All those mechanisms are pro-inflammatory, and they probably contribute together to this slow accumulation of inflammatory damage during aging.
What is the role of nutrition? I think it’s much less clear, but obviously, your microbiome is very important for the integrity of your gut membrane. This is one of the areas we’re very interested in – to understand the role of the microbiome in health in general.
Let’s move to another very popular topic – ketosis and ketogenic diet. Could you briefly explain how ketosis works and why it is beneficial?
Ketosis is a state in which your body accumulates what we call ketone bodies, and there are three types of them – acetate, which is a volatile ketone body, acetoacetate, and, finally, the most important one is beta-hydroxybutyrate, or BHB.
These ketone bodies are predominantly made by the liver from fat, and they accumulate under several circumstances. The most common one that’s been studied for the longest time is fasting. If you fast for 24 hours, your body will start relying on fat from your adipose tissue. This fat will be transformed by the liver into ketone bodies.
We know that BHB is a form of energy, like glucose or fat, and it becomes the predominant form of energy that your body uses during fasting. The two organs that love relying on this form of energy are the brain and the heart.
We published a paper about ten years ago showing that BHB is not just a form of energy but also a signaling molecule, an inhibitor of HDAC, which makes it an epigenetic regulator. We showed in that initial Science paper that BHB induces a state that protects against oxidative stress. This directly links BHB to aging. We found that interesting: not only do you make a new form of energy when you are in ketosis, but this new form of energy also acts as an antioxidant.
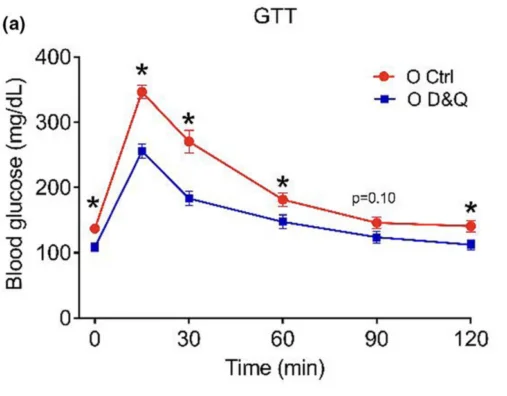
That led us to a simple question: could this be a way to increase lifespan or healthspan? With a postdoc at the lab at the time, John Newman, who is now a faculty member at Buck, we did a lifespan study with mice on ketogenic diet. We were able to show a significant increase in healthspan, particularly in terms of brain function, and a minimal increase in lifespan.
Another group at UC Davis, directed by John Ramsey, published right about the same time, and we were in touch with each other. Their paper showed a clear increase in lifespan. The reason they saw a stronger effect on lifespan is because they had the mice continuously on a ketogenic diet, while we did two weeks on, two weeks off. But all the results suggest that this diet has an anti-aging effect.
So, we’ve been really busy doing two things: first, trying to understand how does this work? I told you about epigenetic regulation, and I think it’s one of the mechanisms, but there are other mechanisms. For instance, we know that BHB inhibits the inflammasome, which is one of the major drivers of inflammation. This is, by the way, one way to link nutrition to inflammation and aging.
I told you that one of the ways to enter ketosis was fasting. This takes many different forms: intermittent fasting, time-restricted feeding, calorie restriction. All these states induce ketosis, but there are other states, unrelated to fasting, that also allow you to enter ketosis. One of them is carbohydrate restriction. If you really cut down on carbohydrates, you will enter ketosis.
This is, basically, the idea behind keto diets?
Exactly. Ketogenic diets have generated a lot of interest in the press because people tend to lose weight with them. It also decreases insulin secretion, which is one of the major pathways that regulate aging. This just makes a lot of sense that if you quiet down insulin action, this will slow down inflammation, increasing healthspan and lifespan.
The problem with the ketogenic diet is that it’s hard to follow. You are only allowed to eat 15-20 grams of carbohydrates per day. That means an apple, and you’re done. No pasta, no bread, no pizza, none of the other things that we all like.
So, we developed an alternative way to enter ketosis via ketone body esters. We’re talking about a molecule of BHB derivatized with another molecule that allows it to be ingested and generate a state of ketosis.
This is already sold as a supplement, but the problem is it tastes terrible. We’re working on second-generation ketone esters that will taste a lot better. This will help more people to explore the whole world of keto.
The question is, do we really need the ketogenic diet to benefit from ketosis, or is it sort of a blunt instrument where we restrict ourselves quite a lot in what we eat, maybe even causing ourselves some harm, when we have all kinds of fasting, and your supplement on top of that?
What is the relative value of a ketogenic diet vs intermittent fasting vs the supplement? We just don’t know yet. It would be amazing if the supplement would recapitulate all the effects of a ketogenic diet, but I suspect it might not, because carbohydrate restriction is probably beneficial in itself.
We are contemplating studies that would compare those interventions head-to-head using biomarkers of aging. I would argue that at this point, you could actually rotate between them, maximizing your chances that one of them is going to work.
There’s some interesting emerging evidence that a ketogenic diet does not have to be followed continuously. In our study, we did it intermittently. I’ve heard rumors about groups doing even shorter periods of ketogenic diet and seeing significant effects. So it could be that you only need to be on a keto diet for, say, three days a week, and you would still get all the benefits.
One question about carbohydrates: what about fruits and berries?
That’s an important point. I was on a ketogenic diet for extended periods of time, and I’ve always found it hard because I was craving fruit. There’s something delicious and wonderful about fruits, and I admit I was craving them.
If you look at fruits, there’s a whole hierarchy of how healthy they are, at least based on the science of aging. Possibly the worst thing you can do is to drink any fruit juice. Many people drink a glass of orange juice every morning thinking that they’re doing something healthy for themselves. But it’s actually full of sugar, rapidly absorbed, and hence not healthy.
On the other hand, fruits contain many phytonutrients that are firmly linked to health – flavonoids, polyphenols, anthocyanin – all kinds of molecules that we know are beneficial. The question is, what is the best way to get them? This is where berries come in. Some of them are highly colored, which means they contain a lot of phytonutrients, and many of them are also relatively low in sugar. These are the only fruits that I’m eating.
They are also delicious.
They are indeed. And they allow you to minimize the carbohydrate intake while still getting many of the phytonutrients.
Something that recent research shows rather clearly is the importance of post-meal glucose spikes. Is it possible to temper them with supplements such as the one you were talking about?
This is a very interesting question. There’s an observation we’ve made but not published, that post-meal glucose excursions appear to be even more predictive than your hemoglobin A1C (HbA1C) of macrovascular disease, heart attacks, and strokes. We don’t really know how that works, but maybe it’s linked to the spike in insulin.
So, it’s not so much your average blood glucose that’s important, but the height of your post-meal spike. Two things are crucial here. First, what types of carbohydrates do you eat? Are those “fast carbohydrates” or the healthier kind? Second, in what combinations are they eaten? For example, if you eat a piece of baguette by itself, you’re in for a very large spike, but if you dip it in olive oil, this will delay gastric emptying, and the same amount of carbohydrates will probably result in a smaller spike.
I always advise people to use CGM, continuous glucose monitoring, for at least two weeks or a month to see the patterns. The response is highly individual. I might spike with French toast, but you might not. I might not spike with a banana, but you might. We think that one of the factors that determine this is your microbiome, and the only way to detect it is CGM.
So, you wear this continuous glucose monitor, while exposing yourself to many different foods such as fruit, in order to determine what makes you spike. When I did this, I found out that two of my favorite fruits, dates and figs, were horrible for my blood sugar, and I stopped eating them. I also saw that raspberries and blueberries do not affect my blood sugar. So, this is an area where I would encourage everyone to experiment. Just ask your doctor to prescribe it for two weeks, and you’ll get a lot of data.
One interesting thing we found was that if you take a rapidly absorbed carbohydrate and you mix it with the ketone body ester, this suppresses the glycemic response. It’s unpublished but other people have shown it too. We don’t fully understand the mechanism, but I think it’s potentially very important.
Unlike with, say, the Mediterranean diet, we obviously still don’t have epidemiological data on keto diets (as unreliable as epidemiological data can be). How sure are we that the ketogenic diet doesn’t have long-term deleterious effects?
The short answer is we are not. But we can infer from data in mice where we see significant effects on healthspan and lifespan that the same diet is likely to have the same effect on humans, although it’s not proven, and it’s important for people to know this.
I am encouraged by the fact that many of the markers that we know are associated with accelerated aging, such as increased inflammation, sugar spikes, and so on, tend to be alleviated by the ketogenic diet or by the ketone body ester.
Still, the point you’re making is important, because of the principle “do no harm”. So far, the markers in short-term studies look good. However, at least one version of the ketogenic diet, the Atkins diet, is rich in saturated fat, and I think it’s clear that this particular diet should be avoided, because it’s highly pro-inflammatory.
But when we think about more balanced diets, such as the ketotarian diet, or intermittent ketosis, I’m much more comfortable with the idea that you can do it for a long time without much risk to your health.
But there is some concern about the LDL levels in people on ketogenic diets. Could you address that?
I think this is totally valid. The ketogenic diet, even in its better forms, is associated with an increase in LDL, and that is a potential risk factor for heart attacks and stroke. Several groups have extensively studied people on ketogenic diets. I’m thinking of a company called Virta Health, which does a lot of clinical trials. I know they are seeing this increase in LDL, but I don’t think they’ve seen an increase in heart attacks.
These are complex interventions, so we need to do lots of experiments and we also need to account for variability. What might be a healthy diet for you might not be as healthy for me. If I already have high cholesterol levels, or a family history of heart disease, I’d be more cautious.
What about exercising during that 16-hour window when you’re on intermittent fasting?
It depends on the type of exercise. For me, if it’s an endurance exercise, like going for a two-hour bike ride, or for a run, I can easily do it when fasting, although it clearly requires some adjustment. Once, I brought a friend with me on a two-hour bike ride, and this friend had just started fasting. After about an hour, we had to stop, because he got dizzy. So, it’s not something you can start right from the beginning, but I think exercising while fasting is good because it accelerates ketosis.
But if you’re going to do weightlifting or sprinting or any kind of exercise that is anaerobic, or glycolysis-dependent, the muscles that are necessary for this type of exercise rely on glucose and glycogen. When you’re fasting for a long time, your glycogen stores get depleted. So, those types of muscle fiber will be craving what they need, which is sugar. When I have a session of weightlifting, I try doing it more towards the end of the day when I’m fed, and that also would be my recommendation.
A couple more questions about the Buck. I really appreciate the fact that you explore the social aspects of longevity, including reproductive aging, so could you please tell us more about it?
We created this new Buck Center for Female Reproductive Longevity, and a consortium as well. The center is a group of scientists within the Buck, including my lab (where we work on NAD and reproductive aging). The idea is to address something that has not been really studied scientifically. Why is the ovary one of the first organs to age? In this regard, the ovary is a bit like the thymus. And it doesn’t seem like it has to be, because humans are one of the only organisms that have this trait.
We have got significant funding from Nicole Shanahan, who has helped us to build the center and the consortium. The latter is the same effort, but it’s directed towards every non-Buck scientist. So, if you work somewhere else in the country, you can request funding.
This has created a lot of interest in the field, and I hope that in the future, it will lead to several things. First, by the age of 30, 10-15% of women are already infertile. As women enter the workforce and develop their careers, many of them are delaying childbearing. As we live longer and longer, I suspect this tendency will only grow. If you’re 35 and pregnant, this is called “geriatric pregnancy”, and that sounds scary. We are trying to address this as an unmet medical need.
Another reason for doing that is that after menopause, we see acceleration of aging, so if you can delay menopause by a few years, you can expect this to lead to an increase in lifespan and healthspan. Many other areas of female biology have also been largely ignored, and we are very excited to be a leader in this field – to basically help build a new field.
The Buck is sort of isolated, detached, both literally and figuratively. It even looks like a secretive facility that develops ways to rejuvenate wealthy people – although I know this is not true. How would you convince a regular person that you work for them?
This isolation of the institute has certainly contributed to people having all kinds of conspiratorial thoughts, like “they are probably doing something that should be hidden”. I’ve been trying to fight this in multiple ways. Our science is for everyone. Of course, we are interested in increasing longevity, but we also have a society where we see increasing disparity between the educated and wealthy people and the rest.
We really need to address longevity in all populations. Pushing for extreme longevity is fascinating, and that’s where the science leads us, but there are so many other things that we can do to understand what a healthy lifestyle is, and why aging trajectories are splitting in two, with the wealthy and educated living longer and longer and the rest of the population living shorter and shorter.
Our mission is directed towards both of those goals. I’m equally excited about pushing the envelope and looking for new drugs for extreme longevity as I am by understanding the life factors that separate those two groups of the population.
If you are a minority, even living in Marin County (where the Buck is located), why is your lifespan much shorter than that of the rich? For me, that’s an extremely important question and a challenge. I hate this idea of our field being “medicine by the wealthy, for the wealthy”. So, we are currently fundraising for a new project we call the Healthspan Institute with a whole new building that will allow us to really delve into these questions and focus on the populations that currently have shorter lifespans.
We would like to ask you a small favor. We are a non-profit foundation, and unlike some other organizations, we have no shareholders and no products to sell you. All our news and educational content is free for everyone to read, but it does mean that we rely on the help of people like you. Every contribution, no matter if it’s big or small, supports independent journalism and sustains our future.






 There are at least two species in the animal world whose lifespans have been naturally extended far beyond the lifespans of their close cousins. These animals are the naked mole rat and Brandt’s bat. Here is what we know about how this increase of lifespan has happened.
There are at least two species in the animal world whose lifespans have been naturally extended far beyond the lifespans of their close cousins. These animals are the naked mole rat and Brandt’s bat. Here is what we know about how this increase of lifespan has happened.
 We tend to feel anxious when we encounter something new, like the idea of intervening in the aging procesess. Part of this reaction is biologically programmed, as during human evolution, new things might turn out to be dangerous; another part is related to the deficiency of knowledge about the new interventions and the indirect consequences of their application.
We tend to feel anxious when we encounter something new, like the idea of intervening in the aging procesess. Part of this reaction is biologically programmed, as during human evolution, new things might turn out to be dangerous; another part is related to the deficiency of knowledge about the new interventions and the indirect consequences of their application.