Professor João Pedro de Magalhães leads the Genomics of Ageing and Rejuvenation Lab at the Institute of Inflammation and Ageing in the University of Birmingham. He is also CSO of YouthBio Therapeutics, a US-based biotech company that develops rejuvenation gene therapies based on partial reprogramming by Yamanaka factors. Last year, he co-authored The hoverfly and the wasp: A critique of the hallmarks of aging as a paradigm. Here, we discuss this critique and other fascinating geroscience-related topics.
Most mature scientific fields have a unified theory, but geroscience doesn’t. Why is it important for our field to have such as theory?
We don’t have a good understanding of a lot of complex diseases, particularly quite a few age-related diseases. For instance, we don’t know what causes Alzheimer’s. Of course, once you understand what causes a certain pathology or a biological process, that makes it a lot easier to intervene in it.
Infectious diseases are probably the best example. If you understand that AIDS is caused by HIV, then you can try targeting HIV to prevent AIDS. Having a pathophysiological, mechanistic understanding of the causes of a given disease allows you to better develop therapies.
That’s why it’s important to have a biological understanding of aging – so we can better intervene in it. One of the biggest questions in the field of aging is still “Why do we age?” There are several theories, or hypotheses, but none of them have been proven yet.
In your recent paper, you offer an interesting, and I think pretty convincing, critique of the hallmarks of aging paradigm, or a false paradigm, as you call it.
The hallmarks paper was a great summary of the field, and if you read it, the authors are fairly cautious about it. It’s a set of hypotheses, but people might have taken the hallmarks of aging a bit too seriously – as the dogma, the Bible of the field, and that’s not what it is.
It’s a great review. But it’s not a paradigm, it does not explain aging. In fact, for decades, we’ve been in a situation where we don’t have a good mechanistic explanation of aging. Again, there’s a lot of hypotheses, and some may turn out to be right, but they may all turn out to be wrong as well, that’s a possibility.
We should focus on really understanding aging, but I feel we’ve shifted focus a bit in that regard. There’s a lot of focus on longevity interventions (and that’s exciting as well), but not so much on understanding why we age, on discovering the underlying mechanisms of aging.
Some scientists hold the opposite view – that we should focus on finding anti-aging interventions, and that might give us clues about why we age.
I would disagree with that. You can have interventions that you don’t understand how they work. We know that aspirin works – it reduces pain, inflammation – but we don’t really understand how it works. So, even if you have an intervention that extends longevity, figuring out how it works is not trivial.
I would agree that interventions, i.e., ways of changing the aging phenotype, are important for us if we want to study the mechanisms of aging. For example, caloric restriction is important because in most model systems, it extends lifespan and retards aging, which gives us a model for studying the mechanisms of aging: you’re going to have experimental groups of animals that live longer than others, and you can then ask questions like: why do these animals age at different paces?
In that regard, I do think that interventions and longevity manipulations can provide insights, because they provide this diversity in the rate of aging that can help us understand its mechanisms. But, given that we know of lots of interventions already, I don’t think you necessarily need more interventions. You can try to figure out why certain interventions work but not necessarily try to come up with more interventions. In model systems, we have already discovered different longevity manipulations.
If I go to our DrugAge database, it has over 3000 entries, over a thousand drugs. So, we already know over a thousand drugs that work (admittedly, a lot of this will be for invertebrate, not mammalian, models). So, we know quite a lot already in terms of interventions, but in the vast majority of cases, we actually don’t know how they work.
Could you elaborate on what you call in your paper the false distinction between aging and the diseases of aging?
The relationship between aging and age-related diseases has been debated for decades. I think it’s more semantics than actual biology. It depends on how you define aging. I would say that aging is a process that predisposes us to a variety of diseases. There are overlapping mechanisms between age-related diseases. For instance, cancer and neurodegenerative diseases have this overlap, although there are also mechanisms that are specific to cancer and neurodegenerative diseases that don’t relate to other age-related pathologies. The overlap is partial. I would say that if we can understand the underlying aging process that predisposes us to various diseases, that would allow us to better understand how to intervene in aging and hence in age-related diseases.
We have drugs like rapamycin that seem to alleviate many age-related pathologies. How do such drugs fit into this picture?
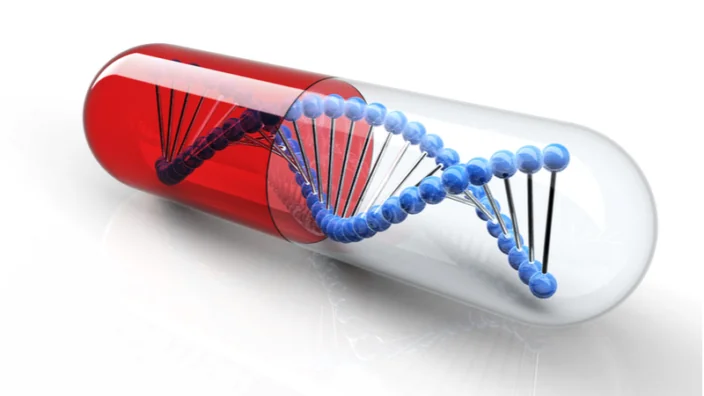
On one hand, longevity drugs are a fascinating and important topic. Whether a drug can slow down human aging is another big question. As I mentioned, we know over a thousand drugs that can extend longevity (not necessarily slow aging) in model systems. So, there’s a big space in terms of longevity pharmacology that potentially can lead to clinical applications in humans, which would be fantastic.
Rapamycin fits very well into that. It’s quite well-studied. It extends lifespan in mice quite robustly. It is one of the most promising longevity drugs. We have some mechanistic understanding of rapamycin, because, well, TOR, which is “target of rapamycin”, but TOR does quite a lot of things.
I don’t think we fully understand at the mechanistic level how we go from rapamycin inhibiting TOR to retarding aging. From a clinical applications perspective, the development of TOR inhibitors and rapalogs with fewer side effects is a very exciting area of study.
Another interesting distinction I heard in one of your talks is between slowing and reversing aging. Do we have any proven interventions that actually reverse aging in complex models?
You could argue that there are some really simple model systems where we can reverse aging. You could also argue that we can reverse aging in human cells with telomerase and cellular reprogramming with Yamanaka factors, but whether that applies to whole organs is a completely different question. The jury is still out on whether we can actually reverse aging in mammals.
I think this might be a terminology issue. If you take an obese individual, and this individual goes on a diet, they will be healthier. Their risks from various age-related diseases are going to decrease because of the diet, but that doesn’t mean that this person has been rejuvenated, it just means that a lifestyle intervention improved their health.
A lot of times, you can have interventions that improve health and maybe ameliorate elements of epigenetic clocks without necessarily doing anything about the process of aging. I think we’ve had this problem in the field for quite a long time – that you can have interventions that increase longevity without necessarily retarding aging, just because they’re healthy. Do obese individuals age faster? I wouldn’t readily assume so, although some of my colleagues may disagree with me.
You can have interventions, pharmacological interventions, for instance, that extend lifespan, but don’t slow down aging in humans and even in model systems. Mice mostly die of cancer, and if you have a drug that prevents cancer, the mice are going to live longer. It doesn’t mean aging has been retarded, even though longevity has increased.
The problem we have in the field is what do those various interventions mean? Do they really slow aging, do they reverse aging, or are they just healthy? That’s why we sometimes need to be more careful about what we are claiming to have achieved.
How would you show something like aging reversal? To me, there’s still a question mark on it. I think you must have some pretty strong evidence for it – functional evidence, molecular evidence. It has to be something quite substantial to prove that you’ve reversed aging in a mammalian organism, that you’ve rejuvenated a tissue. I think that would require some pretty substantial evidence which I haven’t seen yet. Going back to your question, in complex models, such as mammals – no, I don’t think we have really reversed aging.
You probably don’t think that biomarkers of aging, such as epigenetic clocks, can give us the definitive answer, right? For instance, the thymus rejuvenation study – was there rejuvenation or not?
In the thymus rejuvenation paper, my recollection is that they didn’t have controls, a placebo group. That’s a big problem. If you don’t have controls, who knows what else those individuals are doing? I believe they’re trying to do a bigger study. Hopefully they will do a follow-up that will validate that, but going back to epigenetic clocks, I think there’s still a lot of question marks about what they are actually measuring. We don’t understand their mechanistic or biological basis.
Just recently, there was this paper showing that patients with COVID-19 show accelerated aging if you use epigenetic clocks. That’s interesting, but maybe that means that the clocks are just looking at inflammation? That’s a possibility. If you get an infection, of course you’re sick, and your clock would go up because of the inflammation, of the immune response.
This doesn’t mean you’re aging faster or that your biological age has increased. It just means you’re sick. When you recover, you’re not infected anymore, your clock goes down, but that doesn’t show rejuvenation, it just means you don’t have an infection anymore.
I think this shows one of the problems with epigenetic clocks in that we don’t really understand what they’re measuring. If they’re measuring health, that’s interesting as well, and of course, that would inversely correlate with aging, but it’s not the same as measuring biological age, it’s measuring how healthy an individual is, which, again, can be influenced by things like infections, or being obese and then going on a diet.
We still don’t know that. I think epigenetic clocks are fascinating, and their accuracy is very impressive. I did not expect clocks to become so accurate, I have to say, I was very impressed and surprised with that, but we still don’t understand what’s the biological and molecular basis behind them.
From the bioinformatics point of view, that’s not necessarily a question we must ask ourselves. If we see a strong correlation, we can just keep using this as a tool.
We can, but I would push back here as a bioinformatician: particularly if we are using human data, we have to be very careful about the correlations we find, because with humans, you can’t really control. If you’re experimenting on animals, you can keep them in a cage, they all have similar genetics, they eat the same food.
People, on the other hand, vary a lot. You can find all kinds of correlations, like wealth correlates with longevity, and rich people tend to live longer. Does that mean that money slows down your aging process? No, it just means wealthier people tend to live healthier lives.
People from the bioinformatics field, in my experience, are mostly okay with this black box approach. It’s like, we have our big data, we see correlations, that’s all we need.
I think that depends on the application. Epigenetic clocks are fantastic for some things. I know people use them to test interventions, to do studies in different species, studies in wild populations of animals, when they don’t know the age and they use epigenetic clocks to determine that.
In that regard, it’s a fantastic tool, and you don’t need to understand how it works, but if you are asking whether you’re rejuvenating an individual, and you’re using an epigenetic clock to answer that question, then you need to understand a bit more about this clock, about the markers and the readouts you’re using. That’s when it becomes more important.
As a scientist, I’m always curious, how does this work? What cell types are contributing to the clock? What genes, molecules, enzymes, mechanisms? If you can figure out how the clocks work, you may be more able to devise ways of affecting them. You can develop interventions. So, for certain applications, you don’t need to know how it works, but for others, biological understanding becomes important.
Let’s take genetic associations. You can find very statistically significant genetic associations, and that’s interesting, but you also want to know the molecular mechanisms behind it. Having a statistical significance association doesn’t tell you the whole story. Particularly if you want to take the next step, which is to reverse-engineer a process in order to tweak it, you must have a mechanistic understanding of that process.
That brings me to a question about your work. You have studied long-lived mammals, analyzing their genomes – animals like the bowhead whale and the naked mole rat. What have you learned from studying them?
I see studying long-lived species and the differences between species in terms of lifespan and disease resistance as a complimentary approach. Going back to what I said at the beginning, you need variation in order to study a particular biological process. So, we have variation within species – we have caloric restriction, pharmacological interventions, different types of manipulations of aging.
That’s important: if you want to study mechanisms, if you want to try to understand a process, you want to see how we change it. If you’re studying a disease, generally you study individuals with the disease, individuals without the disease, individuals with different severity of the disease.
If you’re studying a biological process, you want to study different paces of that process. You can do it within species, which we do already, and then a complementary approach is cross-species, because mice age 20-30 times faster than human beings, while some species of turtles and fishes don’t appear to age at all. So, you have a very big spectrum of paces of aging. That gives you diversity in the process of aging that allows you to gather insights.
Of course, if you’re looking across species, the problem is that there’s a lot of other differences. If you’re studying caloric restriction in mice, there’s not that many differences between them, apart from that intervention that you’re studying. On the other hand, if you’re comparing a naked mole rat to a mouse – yes, there’s a difference in lifespan, but there’s also a lot of other differences between them. That’s the difficulty.
We and others have looked at animals like the naked mole rat, the bowhead whale, there were some great recent papers on rockfishes. We published a study last year on the Capuchin monkey, which is a small, long-lived primate. I guess the main message is that you see different genes in these species, but they tend to fall into similar categories, similar pathways.
My overall impression is that when a species evolves longevity, when it is selected for longer lifespan, species tend to use different tricks to achieve that, but these tricks tend to fall into some common themes like tumor suppressors, DNA damage responses, protein homeostasis. There are common themes for how species optimize pathways and processes to extend lifespan.
It is known that if we theoretically could eradicate cancer in humans, that would only extend lifespan by about three years. I guess that’s also true about other species. So, long-lived species must have developed several mechanisms at once, right? There are several tricks up their sleeves?
That’s right. It’s not just one trick. We’ve only really scratched the surface as far as these tricks are concerned, because there’s a lot of differences between species at the genetic level. When you do a comparison between genomes of different species, you’re going to find a lot of differences, and then you can use statistical methods to try to prioritize them.
Through different bioinformatics methods you can try to infer which genes are more important for longevity. You’ll find some clues, but really that’s just the tip of the iceberg. There’s probably a lot we don’t really know in terms of mechanisms that relate to species’ differences in aging, in lifespan. As you say, it’s not just one thing, there are going to be different types of adaptations for life extension in different species.
It’s quite remarkable. If you think about humans and chimpanzees, we are not very different on the genetic level, yet we live considerably longer than chimpanzees, we appear to age slower than them. Which genes are responsible for these differences in lifespan between humans and chimpanzees? It’s not just one thing, but it’s also not an infinite number of things. It’s a finite number, and this number cannot be too big, because there’s not that many differences between humans and chimpanzees. This is an interesting way to look at things.
I think differences in aging between species remains one of the big open questions in the field. Trying to figure it out can also help address the question why we age. We’ve really only scratched the surface as to what is the genetic basis of interspecies differences in age.
It is important to continue in that direction, right?
Absolutely. It’s an important complementary approach. In our lab, we’ve done work on different traditional model systems such as worms, we’ve done some work (mostly with collaborators) on rodents, including with the ITP of the NIA. That’s all interesting, it gives you one line of evidence, because it’s very difficult to study aging in humans.
We’re reliant on short-lived model systems, but they have their own limitations in what they may be teaching us about aging. I would say only a part of it will be relevant to humans, and we’re not sure what part.
On the other hand, we have these long-lived, disease-resistant animals like naked mole rats, whales, Capuchin monkeys, and they can provide a complimentary set of insights and information. That’s why this is important.
Have you seen this new paper that generated quite a lot of buzz, about the rate of somatic mutations and its correlation with lifespan in various species?
I think it’s a fantastic study. It really shows what has been theoretically expected but not really demonstrated in practice, which is that long-lived species accumulate somatic mutations slower than short-lived species. I think, this is primarily due to tumor suppression mechanisms. The question of how relevant this is to other aging pathologies, or aging-related physiological changes, remains to be determined. But it showcases how, if you are evolving long lifespan, one of the things you need to curb is the number of mutations. The data we’ve had so far is mostly from mice and humans, so this is quite an interesting expansion in the repertoire of species.
Another part of your work has to deal with cellular reprogramming, right?
Yes, I’m working with the company called YouthBio, which focuses on cellular reprogramming. I guess we’re not the only company focusing on cellular reprogramming nowadays. We actually were in stealth mode until recently.
Our goal is to develop gene therapies based on cellular rejuvenation and partial reprogramming with Yamanaka factors. It’s a quite interesting topic in itself. As we touched upon already, it does work on cellular models, but there’s still a lot of questions of whether it could work on whole organisms, or how we can make it safe because, of course, reprograming can induce cancer.
As to having bigger, better-funded competitors, I actually don’t see that as a problem. You don’t want to be the only company in a particular field. That’s usually a bad sign. You want to have other companies working in the same space. It shows that this is a dynamic field, a dynamic approach.
Personally, I’m used to always being the underdog. Our lab is not the best funded in the world. There are many bigger, better-funded labs than ours. I’ve always liked that role of being the dark horse and having to compete with bigger labs. I think that helps in a lot of circumstances.
So, the fact that there are much bigger companies working in the same space is not necessarily a problem. It shows the enthusiasm about this particular approach. It also means that if we can make it work, it will have a lot of value, and a big company might buy our technology and knowhow.
Calico is one particularly big and well-funded company that has been around for a long time. Do you know if they have had any breakthroughs in reprogramming?
Not really. They’ve published some nice papers, but certainly, for the amount of funding they have, although you never know what they can come up with, I would say, so far, they’ve been fairly disappointing. When there’s a company with billions of dollars, you expect it to be a leader in the field, to deliver breakthrough after breakthrough.
That’s not happened; they’re not leaders in the field. Yes, they do some nice work, but so far, they haven’t really delivered what nearly everyone expected when they started, and it’s been nearly 10 years. I think it’s fair to say that they’ve been disappointing, unless they come up with something amazing. You never know.
The question is do you maybe see their lack of progress as a sign that cellular reprogramming might be a dead end?
In terms of Altos, NewLife, and Retro, all those big companies working on cellular reprogramming – yes, it could blow up in their faces. I think the best analogy is telomerase. I remember when telomerase came out and it could prevent cellular senescence and rejuvenate cells.
In vitro, telomerase was fantastic. And people were talking about telomerase therapies, curing age-related diseases, reversing aging. It hasn’t really happened, and there are reasons for that. One, because telomerase by itself doesn’t really slow down aging. It prevents aging at the cellular senescence level, but it doesn’t prevent other aspects of aging in vivo. It also has certain risks in terms of cancer, et cetera. The point is that something that worked very well in vitro in terms of preventing aging, in this case telomerase, hasn’t so far worked in organisms, much less in the clinic.
The same could happen with cellular reprogramming. This is a possibility we have to be prepared for. On the other hand, we don’t know yet, and reprogramming has a bigger impact on cells than telomerase. I would be surprised if Yamanaka factors by themselves worked without side effects, but there may be ways of tweaking reprogramming, and that’s some of the work we’re trying to do – to make it more efficient and safer.
Now, maybe it does work, not necessarily at the level of rejuvenating human beings, but maybe it has applications in certain conditions. As I’m sure you’re aware, there’s a lot of interest in reprogramming for regenerative medicine – not rejuvenation, but just regenerative medicine in patients with spinal cord injuries or other conditions that may benefit from reprogramming.
Maybe in ovarian aging.
Exactly. So, there may be specific applications. Even if it doesn’t pan out, if we cannot reverse aging in human beings with programming, maybe it will still have some clinical applications, as a lot of companies even outside of the field of aging are already exploring.
The fact that not just Altos, but several big companies are investing in the space means we’re probably going to have an answer to it – whether it works or not. This would be very beneficial because even if it doesn’t work, if reprogramming is a dead end and we’re just wasting our time, we want to know about it sooner than later, because we want to move on to other things.
We’d also want to have at least one single breakthrough rather sooner than later, so to not scare off the investors.
Yes, absolutely. We need a success story in the field of aging. We still don’t have one. We don’t have a therapy that actually works in human beings. I’m somewhat skeptical that reprogramming is going to be that first success story, because I think the pharmacological approach has better chances as folks have been doing drug development for a long time.
There’s a bunch of companies working on pharmacological approaches to aging, doing clinical trials for senolytics, for caloric restriction mimetics, and some of those approaches might work. Most of them will fail, but hopefully at least one will work. If we can have a success from a pharmacological approach, that would be fantastic.
I would disagree however with your assumption that without a success story, the investors are going to be disappointed. Why? Because people are not getting younger, that’s the bottom line. The incidence of age-related diseases is going to increase. The graying of the population worldwide is going to continue. That’s why we’re going to have more and more motivation to intervene.
We had, I would say, quite a disappointment some years back with resveratrol. You might remember the resveratrol debacle. There was a lot of interest, they were purchased for a huge sum, a lot of excitement, but then it didn’t work out.
You might have expected a big disappointment to hurt the field, but that’s not what happened at all, quite the opposite. The field has flourished. So, we can have some flops. However, if we have a lot of them, that might be an issue, because there are different types of investors. There are investors that believe in the philosophy of life extension, of reversing or at least retarding aging. Such investors are going to stay, no matter the difficulties.
You have a different class of investors that appeared more recently, and they see aging and the longevity industry as a way to make money. If there’s a lot of flops in the field, if many companies fail in a short period of time, I can see those investors going elsewhere.
I agree about the “gray tsunami”. Maybe in this case, governments should step in much more massively, increasing the amount of spending dramatically, because it’s still laughingly small?
Absolutely, but you’re preaching to the converted. We need more government funding for aging. In a way, government funding is the main funding we need because that’s the big money. I think the NIA (National Institute of Aging) budget is around $4 billion a year. It’s like an Altos Labs every year. Most of it goes to Alzheimer’s disease, not to the biology of aging. The biology of aging gets a tiny fraction of that. That’s what we need, we need billions of dollars every year from the government.
Having steady government funding allows you to do blue skies research, to address the basic questions we were talking about, like why we age? No company is going to say: Pedro, here’s a lot of money for you to tell us why we age! That’s not going to happen.
For those kinds of basic biology projects, we’re still relying on government funding and charities. The major driver of science discovery is funding fundamental science, which leads to a lot to startups and ultimately clinical applications. But we need that fundamental science to begin with, and it has to be funded by the government and charities.
I really liked your Twitter description that describes you as a “scientist planning to live forever”. I don’t know how serious you are about that, but I really like how unapologetic you are. However, that’s not a popular position today. How would you defend it?
That’s a good question. Interestingly, there’s been a couple of people in recent times telling me that they like my Twitter description. It also means that there are some people who don’t like it, they just don’t mention it to me.
So, first of all, I think sometimes you have to compromise on tactical decisions – on a grant application, in a talk. But don’t compromise on strategy. If your goal is to cure aging, then say it, don’t compromise on it.
When I started in the field, my PhD supervisor Olivier Toussaint, who sadly passed away a few years ago, asked me: do you really want to be going around telling everybody your goal is to cure aging? I said, yes, because that’s the goal. I could pretend not to, like some people do.
I know scientists in the field whose goal is to cure aging who don’t talk about it because they’re afraid they’re going to miss opportunities, and maybe I’ve missed opportunities because of that, I don’t know. But in the end, that’s the goal and there’s no point in faking it.
That doesn’t mean that everyone is going to agree with me or that this is the best way of selling the field. And we’ve had some discussions about it. I think we need to sell the field in different ways to different people. And there are other ways – to call it geroscience, to focus on healthspan. For certain audiences, that’s going to work better than saying we’re going to try to cure aging.
As I said, sometimes you’ll have to compromise on tactical decisions. Ultimately, what I want to do is to cure aging. And, if people don’t like it, then I’m happy to discuss it.
It’s not like we’re making biological weapons. We’re not doing anything wrong. We’re just trying to eliminate age-related diseases – to prevent people from having Alzheimer’s, cancer, cardiovascular diseases. There’s nothing wrong with that.
Having said that, I don’t think we’re going to cure aging in my lifetime. After all, we don’t have anything that works yet. As you may know, I’ve done some work in cryopreservation as well. Here too, I’ve been open about it. I think human cryopreservation is achievable. And it’s important to keep your long-term goals in mind.
It’s about what you want to achieve in your life. Most of my friends at school wanted to be football players. I was never good enough to be a football player, otherwise I would have wanted to be one.
From a very early age, I wanted to cure aging. I thought that the main thing in life is being healthy, and no matter how much money you have, you’re not going to stay healthy if you’re aging. So, I dreamed about working on this topic and that’s what I’m doing now. Even if we’re not going to cure aging in my life, at least we’ll give it our best shot.