A new study conducted by a team of Japanese scientists and published in Scientific Reports details how cells can have their damaged mitochondria destroyed and replaced with healthy ones, offering a potential solution to the problem of mitochondrial dysfunction.
Out with the old, in with the new
In order to destroy the existing mitochondrial DNA (mtDNA) in human fibroblasts, the team engineered a plasmid with XbaIR, an endonuclease that can digest mtDNA. This caused the existing mtDNA to drop to less than 10% of its original value, showing that the vast majority of the mitochondria had been destroyed.
This treatment was followed by an injection of mitochondria from outside the cell. These exogenous mitochondria successfully replaced the existing mitochondria, and 70% of the mtDNA of the treated cells was from the new mitochondria, demonstrating the success of this approach.
Developing an intervention
After proving the concept, the researchers then turned to human fibroblasts with a known disease state. Taking cells from a baby with mitochondrially caused Leigh syndrome, a disease that leads to neurological disorders, they performed the same experiment, attempting to destroy the existing mtDNA and replacing it with new mitochondria.
The results were significant. Cells that had been treated in this way exhibited significantly more uniform, healthy mtDNA than their untreated counterparts. The mutation rate, which was 90% in the untreated cells, dropped to 25% in the treated cells. A total of 60% of the treated cells were fully healthy with replaced mitochondria.
The practical effects took time to manifest, as the treated cells needed to recover from their time with depleted mitochondria. However, after 30 cell divisions, the mitochondrially replaced cells had considerably healthier phenotypes than their unmodified counterparts.
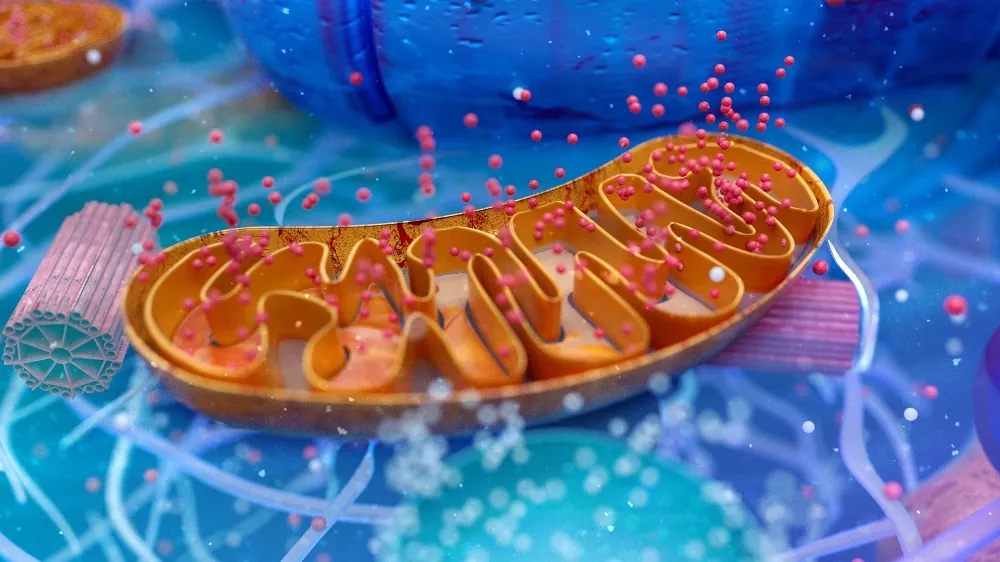
The mitochondria are the powerhouses of the cell, and these cells were able to more efficiently generate ATP, the substance that our cells use for energy. Their mitochondrial respiration was increased while non-mitochondrial respiration was decreased. Their ability to respond to stress was also enhanced; both oxidative stress and starvation resulted in less cell death than their unmodified counterparts.
Enhancing uptake
The researchers then set their sights on ways that cells might be better encouraged to take up donor mitochondria into themselves. When a cell integrates foreign material, it is known as macropinocytosis, and the researchers wished to enhance this as much as was feasible.
What they discovered was very relevant to aging research as a whole. The suppression of the mTORC1 pathway was critical to the uptake of new mitochondria. Cells that had their mitochondria depleted activated the AMPK pathway, introducing the new mitochondria further activated it, and rapamycin, which suppresses mTORC1, was shown to activate AMPK further. Deprived of their energy sources, the cells were effectively undergoing caloric restriction. While the relationship is complicated, this shows a link between caloric restriction, deregulated nutrient sensing, and mitochondrial dysfunction.
Abstract
Mitochondrial diseases currently have no cure regardless of whether the cause is a nuclear or mitochondrial genome mutation. Mitochondrial dysfunction notably affects a wide range of disorders in aged individuals, including neurodegenerative diseases, cancers, and even senescence. Here, we present a procedure to generate mitochondrial DNA-replaced somatic cells with a combination of a temporal reduction in endogenous mitochondrial DNA and coincubation with exogeneous isolated mitochondria. Heteroplasmy in mitochondrial disease patient-derived fibroblasts in which the mutant genotype was dominant over the wild-type genotype was reversed. Mitochondrial disease patient-derived fibroblasts regained respiratory function and showed lifespan extension. Mitochondrial membranous components were utilized as a vehicle to deliver the genetic materials into endogenous mitochondria-like horizontal genetic transfer in prokaryotes. Mitochondrial DNA-replaced cells could be a resource for transplantation to treat maternal inherited mitochondrial diseases.
Conclusion
This cell culture research did not re-introduce the treated cells into a human being, so no claims can be made as to its effectiveness as an intervention. It only performed a preliminary investigation into methods for potentially introducing new mtDNA into existing, living cells.
It may be currently feasible to develop an intervention that uses injections of induced pluripotent stem cells (iPSCs) developed from mitochondrially replaced cells. An intervention that replaces mitochondria in situ, without the need to replace the cells themselves, is still beyond the horizon.
However, we look forward to further investigation on this subject, as an intervention that replaces damaged mitochondria with healthy counterparts may one day be an effective treatment or even an outright cure for mitochondrial dysfunction, one of the hallmarks of aging.