A recent review published in Cureus shows why fecal microbial transplantation (FMT) might be able to help sufferers of Alzheimer’s disease, showing how tightly the gut and brain are intertwined.
Why would this ever work?
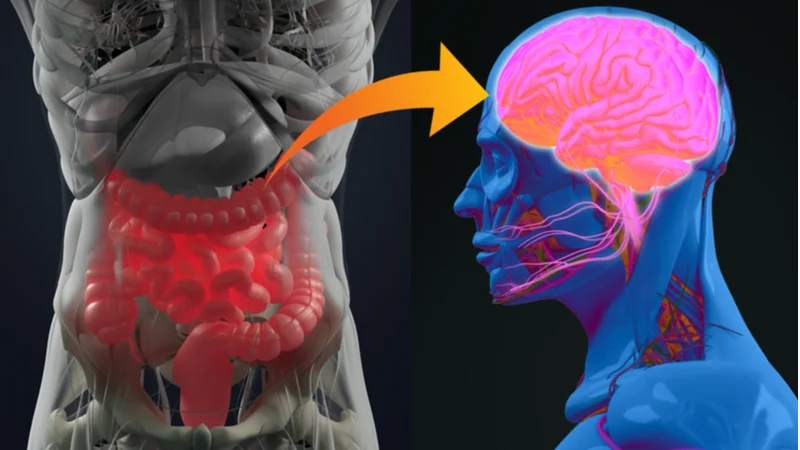
The gut and brain are closely linked through biochemistry, and last month, we published an article about how the gut impacts immune function in the brain. This review notes the associations between gut flora and cognitive health and then takes this idea a step further, collating research showing that gut dysbiosis is a key player in Alzheimer’s disease.
The researchers outline a chain of biological relationships. Gut dysbiosis increases the level of harmful compounds in the gut, decreases beneficial compounds such as short-chain fatty acids, and negatively impacts tight junction proteins, such as zonulin and occludin, which affect intestinal permeability [1] and directly affect the blood-brain barrier [2].
Increased intestinal permeability has a negative impact on inflammation. Bacteria crossing the intestinal barrier have been shown to activate toll-like receptors 2 and 4, triggering the inflammatory factor NFkB and leading to the release of inflammatory cytokines [3].
As the blood-brain barrier has been opened up by the loss of tight junctions, these cytokines lead to immune cells going where they are not wanted in addition to microglia becoming triggered by inflammation, breaking down the extracellular matrix and causing brain cells to suffer dysfunction, triggering the known pathologies of Alzheimer’s disease [2].
With this in mind, several research groups singled out what they believe to be the bacterial culprits in this chain of events. One of the most notable is Bacteroides, which was found to be associated with increased amyloid-beta (Aß) in the brain: the key hallmark of Alzheimer’s disease [4].
Therefore, directly replacing these bacteria in the gut is an approach worth exploring.
The evidence for fecal transplants in Alzheimer’s
The reviewers cite a great many studies showing that FMT, which replaces the gut microbiota with bacteria from another source, may be useful in the treatment of Alzheimer’s disease. Two different mouse studies showed that fecal transplantation, depending on the source, can improve spatial learning and memory [5] as well as performance on the well-known Morris maze test [6].
One transgenic mouse study showed that FMT can decrease inflammatory cytokines, partially restoring the microglia in the brain [7]. Another compelling study also involved transgenic mice, showing that FMT decreased both tau and two different Aß proteins while improving cognitive abilities and increasing neuroplasticity, reflecting the brain’s ability to learn new things [8].
Dietary interventions
While the reviewers do not cite any study showing that a dietary change can ameliorate Alzheimer’s in humans, they do cite a previous review showing that omega-3 fatty acids, antioxidants, a reduced intake of animal proteins, and reduced fat and sugar are linked to a decreased incidence of Alzheimer’s disease [9]. This shows the possibility of prevention rather than a cure. Another team found that long-term caloric restriction can decrease the bacterial culprits involved in the cascade [4].
Conclusion
Fecal transplantation is certainly a disgusting thing to contemplate, but the link between harmful chemicals in the gut and their downstream effects on the brain is supported by substantial evidence. While curing Alzheimer’s disease is an extremely difficult and so far largely fruitless endeavor, preventing or at least delaying Alzheimer’s just might be a far simpler thing to do.
Hopefully, we will soon be able to develop tests and diagnostics that detect people at risk for Alzheimer’s disease, preventing the protein aggregations that are at its core. Before then, eating a healthy diet and maintaining a healthy gut microbiome can be reasonably assumed to be one of the best current approaches to staving off this deadly neurodegenerative disease.
Literature
[1] Janeiro MH, Ramírez MJ, Solas M: Dysbiosis and Alzheimer’s disease: cause or treatment opportunity? [In Press]. Cell Mol Neurobiol. 2021, 10.1007/s10571-020-01024-9
[2] Parker A, Fonseca S, Carding SR: Gut microbes and metabolites as modulators of blood-brain barrier integrity and brain health. Gut Microbes. 2020, 11:135-57. 10.1080/19490976.2019.1638722
[3] Ganesh BP, Versalovic J: Luminal conversion and immunoregulation by probiotics. Front Pharmacol. 2015, 6:269. 10.3389/fphar.2015.00269
[4] Cox LM, Schafer MJ, Sohn J, Vincentini J, Weiner HL, Ginsberg SD, Blaser MJ: Calorie restriction slows age-related microbiota changes in an Alzheimer’s disease model in female mice. Sci Rep. 2019, 9:17904. 10.1038/s41598-019-54187-x
[5] Zhan G, Yang N, Li S, et al.: Abnormal gut microbiota composition contributes to cognitive dysfunction in SAMP8 mice. Aging (Albany NY). 2018, 10:1257-67. 10.18632/aging.101464
[6] Yu F, Han W, Zhan G, et al.: Abnormal gut microbiota composition contributes to cognitive dysfunction in streptozotocin-induced diabetic mice. Aging (Albany NY). 2019, 11:3262-79. 10.18632/aging.101978
[7] Dodiya HB, Kuntz T, Shaik SM, et al.: Sex-specific effects of microbiome perturbations on cerebral Aß amyloidosis and microglia phenotypes. J Exp Med. 2019, 216:1542-60. 10.1084/jem.20182386
[8] Sun J, Xu J, Ling Y, et al.: Fecal microbiota transplantation alleviated Alzheimer’s disease-like pathogenesis in APP/PS1 transgenic mice. Transl Psychiatry. 2019, 9:189. 10.1038/s41398-019-0525-3
[9] Pistollato F, Iglesias RC, Ruiz R, et al.: Nutritional patterns associated with the maintenance of neurocognitive functions and the risk of dementia and Alzheimer’s disease: a focus on human studies. Pharmacol Res. 2018, 131:32-43. 10.1016/j.phrs.2018.03.012