The real cost of life extension advocacy
There is a persistent view that life extension advocacy is something that does not require any investment and can be done in your spare time. Fundraising for overhead expenses is like the proverbial elephant in the room: it is hard not to notice it is there, but people try to avoid talking about it.
The truth is that it all depends on how ambitious the goal of that advocacy is. Without a doubt, talking to friends about the promise of rejuvenation technologies or reposting research news on your Facebook feed is useful and can be done for free.
However, what if the goal is more ambitious – to change local legislation to become more longevity-friendly, to convince decision makers in a government grant system to allocate more money to rejuvenation research, or to reach out to wealthy individuals who can fund more studies? These activities require money. In this article, we will help you become more familiar with the notion of advocacy and the expenditures behind it.
First, let’s make it clear what we mean by life extension advocacy
Advocacy is an activity that aims to influence decision making within political, economic, and social systems and institutions to promote a specific cause and thus ensure positive changes in relation to this cause on multiple levels.
Advocacy implies dealing with the general public as well as academia, business, and government agency representatives who have the formal authority to make policy decisions. The scope of advocacy initiatives can range between regional, national, and global. The suggested changes are usually made on the basis of existing evidence, so data that proves the importance of the problem and the potential of the proposed solution is necessary for successful advocacy.
Life extension advocacy combines two well-known categories: health advocacy (including patient advocacy) and research advocacy.
Health advocacy was born from the early patient rights movement, and today its main concerns involve directly serving the individual or family in order to ensure the fulfillment of their right to health as well as activities that promote health and better access to healthcare for the general public or among specific groups and communities. Public education regarding a specific health issue, such as aging, its social implications, and potential solutions, is an important part of health advocacy.
Research advocacy means efforts to raise public, academia, business and policymaker awareness about the importance of a specific field of research in order to ensure sufficient resources (including funding, workforce and equipment) and a positive regulatory landscape for fundamental and applied research and the development of new technologies. In our case, it is fundamental and translational gerontology that are the focus.
Goals of life extension advocacy
It is probably reasonable to say that every member of our community hopes for rejuvenation therapies to be developed, implemented, and delivered at an affordable price as soon as possible, preferably in their and their relatives’ lifetime. Even though there is steady progress, it would be good to see it speed up. How? Mostly by removing things that are holding us back.
The list of bottlenecks include the following aspects:
Insufficient research funding due to rejuvenation projects being innovative and not well understood by the decision-makers of different funding bodies
Flaws within the grant system: unnecessarily detailed grant applications and reports, making the scientists spend time on them, rigid rules on how money should be used during the project, and delays in funding delivery
Young scientists turning to mainstream topics like single diseases instead of rejuvenation to avoid reputational risks and problems with funding
A need for many more basic studies and unwillingness of business to fund basic science that does not produce a final product that can be sold in order to provide a return on the investment
Local legislation that can be unfriendly towards animal studies or some specific topics of research like stem cells or gene therapy and local legislation that slows down the process of foreign scientific equipment acquisition and delivery
Authors needing to pay high costs to be published in a peer-reviewed journal
Paywalls (paid access to full-text articles) blocking scientific communication and dissemination of knowledge from scientists to the public
Lack of public awareness on the promise of rejuvenation technologies and the positive aspects for our society of their wide implementation
Usage of counterproductive messages by comminuty members, leading to rejection of the idea by the members of the general public
One could call a life extension advocate successful if he or she were gradually removing or mitigating some of these bottlenecks so that the overall situation in the field were measurably improving.
So, what exactly are life extension advocates doing to achieve that? There are three main aspects: study of the field to acquire appropriate expertise, presenting the cause to the public, and internal activities to ensure the widest coverage possible.
An analysis of the field
 For any activity, be it education, fundraising, or lobbying for a new law, a reliable body of evidence should be at hand in order for an advocate to be able to explain and justify suggested changes and initiatives.
For any activity, be it education, fundraising, or lobbying for a new law, a reliable body of evidence should be at hand in order for an advocate to be able to explain and justify suggested changes and initiatives.
Study and analysis can include many focal points, but here are the most important ones for the life extension field. Yes, being a good advocate means to study them all, at least to some extent.
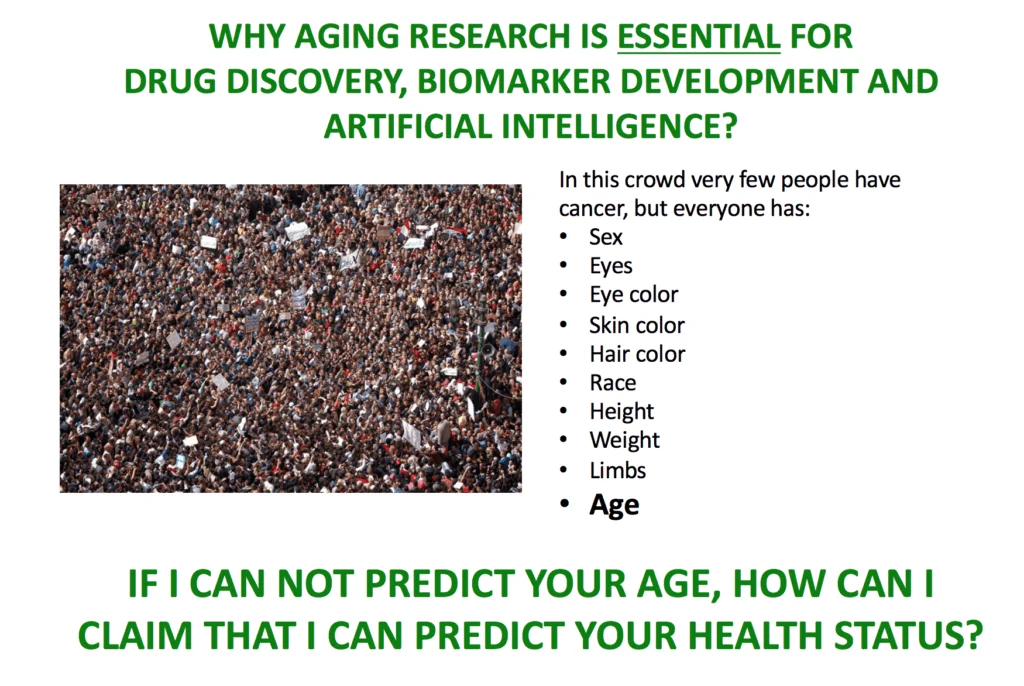
Biological aging as a phenomenon (the hallmarks of aging, the relationship between aging and age-related diseases, the stage of development of different interventions to address different aging processes, data on healthspan and lifespan extension in animal studies, and equivalent data in human studies)
Demography (population structure and dynamics, corresponding morbidity and mortality dynamics both locally and globally, dependence ratio dynamics)
Economy (economic development in relation to population aging, social welfare, and healthcare expenditure dynamics)
Core decision makers, specificially in the fields of healthcare and aging (people and organizations) as well as the process of decisionmaking
Core aging researchers and research organizations (their topic, their progress) along with bottlenecks in rejuvenation research
Global and local policies related to healthcare and scientific activities
The problems of scientific development (decisionmaking in science development, research priorities, the grant system, other sources of funding, the dynamics of funding, scientific publications, and related problems)
The main global and state programs for older persons.
Public perception of rejuvenation research and methods to influence it.
A few examples of the time investment needed to prepare different advocacy materials
To write one popular but accurate article about aging research progress in a specific field, an activist has to spend 2-3 hours to familiarize himself with the latest publications on the topic. Writing 2-3 pages with scientific references can also take several hours. So, one article usually takes a half of the working day.
If the writer is also involved in social media development (which requires posting new original materials every day) this can no longer be considered a hobby: it becomes at the least a part-time job, and that should be paid. Have a look at the level of salaries of scientific writers for financial reference.
To write a large educational article like the ones relating to public concerns about life extension, the activist has to spend about a week to gather appropriate materials from different fields and then has to spend a few days writing the article.
An article on a topic such as overpopulation requires collecting official reports and scientific publications regarding topics such as population dynamics, food production and consumption, water production and consumption, different sources of energy and the forecast for their development, agricultural development, ecology, transportation, comparison of different technologies, and many others. It should be no surprise that one article of this type may need a couple of weeks of part-time activity to prepare.
To prepare a proposal for changes to a law, the activist has to read all related laws (5-10 items that are each 20-30 pages long), find and get familiar with the corresponding body of evidence (for instance, demography dynamics and forecasting), and compose a detailed document covering the propositions of the existing law and suggesting new revisions.
Aside from that, to present these changes at a public event where the law will be discussed, the activist has to prepare a presentation and a speech to inform and engage the audience. Analysis of these laws can take several weeks or even months of full-time work (such a position is called a legislative analyst), and preparation of the document takes at least several days. This does not include the process of lobbying itself; this additional time expenditure will be discussed below.
As you can see, when an activist is deeply involved with advocacy activities, it requires a significant time investment to get familiar with different aspects of our cause that do not really fit into the frame of volunteering. To ensure sufficient progress in the activities involving analytics and writing, an organization has to consider spending money on salaries for its team.
Presenting the cause and networking
 The usual places to promote rejuvenation research and corresponding policies are scientific conferences, public events, and meetings of working groups discussing necessary changes in a law. While the last type of events are most often free (thanks to the principles of democracy), this cannot be said of conferences.
The usual places to promote rejuvenation research and corresponding policies are scientific conferences, public events, and meetings of working groups discussing necessary changes in a law. While the last type of events are most often free (thanks to the principles of democracy), this cannot be said of conferences.
Here are the fees of large conferences that relate to aging and biotechnologies as well as several innovation and VC events to give you an understanding of the expenditures that an advocacy organization has to make to send a representative there (on-site registration for a regular visitor):
The 21st IAGG World Congress of Gerontology and Geriatrics (June 2017): $899
Global Biotechnology Congress (July 2017, Session Speaker Corporate): $1690
Global Innovation Forum (November 2017): €2000
20th Annual Venture Capital + Innovation Conference (February 2018): $350
2018 Aging in America Conference (March 2018): $945
In addition to the fee (which is normally paid way in advance to reduce the cost), going to a conference implies travel expenditures and booking a hotel, which can cost several hundred to a few thousand dollars per person, depending on the region where the conference takes place and its duration. Promotion of a cause on a regular basis means that an organization has to be represented at 10-20 events per year and often even more. Even if half of them do not have a registration fee, it means spending around $10k on the registration and up to $20k on travel and accommodation per person per year.
The truth is, sudden phone calls from charities to the directors of a company (who can make decisions about donations) are most often declined, and mails from charities can be ignored multiple times unless they come from someone whom the director already knows. So, to have an opportunity to talk to a potential philanthropist face-to-face, we have to attend conferences and other public events where we can meet in person.
So, before asking representatives of a life extension advocacy group “Why don’t you guys engage wealthy people to support rejuvenation research?”, it is probably useful to remember these expenditures related to advocacy activities and compare them to the organization’s current budget.
Costs aside, going to a conference for advocacy reasons is a significant workload. First of all, the advocate has to be properly prepared to freely discuss the topic with other participants. Most of the networking, such as talking with decisionmakers, is done during coffee breaks and lunch, which does not leave a chance to rest in between sessions. Gala dinners and culture events for the speakers represent an additional working period during the evenings. Not only are such activities a full-time job, they also require a certain level of mental and physical stamina.
After the conference is over, the activist has to engage in follow-up activities, exchanging emails, preparing new proposals for collaboration, and setting and going to meetings with new partners – or engaging other team members to do so.
In the case of lobbying for changes in the law (which can take several years), the activist has to attend from 5 to 20 meetings of the working group per year to ensure that the proposed changes are still being considered and keep being included in the new version of the law. Each meeting can take a half of a working day and implies some follow-up analytical and networking activities. You can check these links to have an estimate of salaries of professional lobbyists or government relations managers.
Internal activities
As we previously discussed, one of the main bottlenecks in rejuvenation research is funding. Because government and business do not provide sufficient support to these studies, the only alternative source of funding is the general public. However, due to rejuvenation research being a relatively novel topic, not many people know about it and consider it important enough to express their support. This means that activities aimed at dissemination of knowledge are crucial for faster progress.
Educational tool development includes writing popular articles, recording video interviews, writing books, designing infographics, making educational and promotional movies, organizing and broadcasting public discussions and webinars, and hosting conferences. To ensure that this coverage is sufficient to promote the cause, all the materials and all the events should be promoted in social media channels – the development and maintenance of which are an independent part-time to full-time activity.
While a non-profit can engage volunteer support and avoid some (but not all) expenditures on video production and social media management, certain aspects inevitably imply a significant monetary investment.
For instance, organization of a decent scientific conference requires $30-50k (the size of an NIA grant for a scientific conference). This money is spent on booking a conference hall, appropriate sound equipment, arranging meals for the participants, travel and accommodation for the top speakers, translation services, video recording, broadcasting, and technical support.
Editing of the video coming from a one-day conference usually requires a few weeks of part-time work. This is why in case the organization is hosting events on a regular basis, or is producing other video content, it can mean that a video editing specialist should be a part of the core team.
If the conference venue and the list of speakers are not impressive, it is often hard to persuade government representatives to pay a visit, and without that, the interest of newsmakers to report about the event and the cause can be weaker – which, in turn, reduces the impact. This is why while most advocacy organizations look at the costs very carefully, they do not always agree on the cheapest scenario.
The event management, depending on how large the conference is, can require part-time commitment of 2-5 team members for about a year and full-time commitment during the month when the conference takes place. Volunteering in event management is usually not an option: when dealing with VIP participants and partner organizations, it is better to avoid sudden breaks of communication.
This means that, apart from the expenditures of the conference hall and participants’ travel and accommodation, the advocacy group also has to find resources for several part-time salaries for the event managers in order to ensure that the conference will be prepared in time and to a good standard. All of us welcome events where a registration fee is absent, but have you ever thought where else the money for the conference comes from?
It is provided by fundraising for administrative needs (you can check the salaries of fundraisers here), running projects bringing some revenue, or capitalizing on the assets that an organization has (for instance, advertisement on the website); most often, the funds come from all of these activities combined.
Conclusion
Looking at all these costs above, it is really hard to understand why some members of the public expect an advocacy group to effectively promote the cause while also condemning any fundraising efforts to meet these administrative expenditures. Isn’t it more logical to ensure enough resources for a company to operate to its maximum potential in order to have a bigger impact?
American humanitarian activist Dan Pallotta, whose successful campaigns for AIDS and breast cancer research (which later became a case study of Harvard Business School) were explained by significant investments into fundraising activities, was crucified “for greed” and had to go out of business for having spent 40% for overhead while only 5-10% are considered “normal” for a charity. Watch his TEDx Talk to learn this sad story.
Then again, nobody questions the commitment of volunteers. But the studies show that “healthy” volunteering takes no more than 2 hours per week [1], and if it is more, a volunteer can burn out quickly and leave the organization.
This amount of time, even if spent regularly, is not enough to acquire and maintain the necessary level of expertise for networking and lobbying projects. It is also not enough to ensure regular educational activities either.
Life extension advocacy groups are constantly seeking grant opportunities to cover their administrative needs. All of the same problems that impede scientists trying to receive grants for rejuvenation research also impede advocacy projects in our field. Due to the novelty of the idea of aging prevention, not many grant givers are keen to provide resources for its promotion.
So, before you ignore the “Donate” button that you see on the site of a life extension advocacy group, and before you frown at the administrative costs in their annual report, consider this: you and other members of our community are, so far, the only part of population who dislikes aging strongly enough to invest in the solution. The best time to step in is always the same: now.
There is too much work for volunteers to do, and sustained high-quality advocacy and activism comes at a cost; if you agree and want to help us make a real difference, then perhaps consider supporting our work.
Literature
[1] Grant, A. (2014). Give and take: Why helping others drives our success. Penguin books.