Most people interested in rejuvenation and life extension are familiar with Fight Aging!, one of the very first rejuvenation advocacy blogs dating back all the way to the early 2000s; if you’re one of them, then you certainly are familiar with Reason, the man behind FA!.
Over the years, Reason has been a patient yet relentless advocate, acting not only as an information provider for the public but also helping out innumerable organizations and companies in the field of rejuvenation biotechnology in financial and other ways. Back in the day when SRF didn’t exist yet, Reason was a volunteer for Methuselah Foundation; eventually, he helped fund companies such as Oisìn Biotechnologies, CellAge, and LysoCLEAR; and, earlier this month, Reason and Bill Cherman co-founded Repair Biotechnologies, a company focused on gene therapy for rejuvenation, as announced on FA!.
Bill Cherman is an investor in the rejuvenation community who, just like Reason, has contributed to development of many ventures in the field. He is a holder of a gold medal in the Brazilian Mathematics Olympiad, a BA in economics, and a candidate in the Master of Biotechnology Enterprise and Entrepreneurship program at Johns Hopkins. He founded Front Seat Capital, a venture capital firm looking to invest in startups with the potential to change the world.
Repair Biotechnologies, which is presently looking for a Chief Science Officer, will kickstart its activities with a project on thymic regeneration in partnership with Ichor Therapeutics—the creators of LysoCLEAR, Antoxerene, and RecombiPure. The goal of the company, as you can imagine, is to shorten the journey of rejuvenation therapies from the lab to the clinic.
It is extremely heartening to see more and more rejuvenation-focused companies and organizations sprouting and building up to the turning point when this emerging field of science will cease being fringe and become a hot topic not only in the relatively small circle of biogerontology (where it has been one for a while now) but also in business and public discourse. We’re very grateful to Reason and Bill for taking us yet another step closer to the finish line and for answering our questions.
We’d like to ask some details of your story as a rejuvenation advocate. When and under what circumstances did it become clear to you that aging is a problem?
While it would be delightful to claim that I am a rational entity who came to that conclusion through utilitarian thought, in fact, it was more of a bolt from the blue. For no apparent reason, it suddenly came to me one evening that I didn’t want to die – and not in the academic way that most people hold that conviction but a deep, visceral, adrenaline-laden realization of the sort in which one accepts immediately that something important in life has been done and determined, a corner turned. Before that happened, I was no more than passingly interested in aging as a topic, but afterwards… well, I woke up. Of course, that was a long time ago now, far prior to my present understanding of what is plausible and possible, and realization on its own achieves nothing. It took years to learn enough to progress any sort of understanding as to how a non-life-scientist could make a difference.
We have noticed that there has been a sea change in both progress and enthusiasm from the academic community for rejuvenation biotechnology and targeting aging directly to prevent age-related diseases. Have you observed a similar rise in support, and what factors, if any, do you think are driving this?
I think that these things progress in cycles, based on the timescale of human collaboration. It takes a few years to go from desire to setting up an organization, a few years for the organization to get somewhere, and a few years for others to be inspired to their ventures by the organization. Bootstrapping only looks smooth in hindsight. We have been transitioning from one business cycle to another these past few years, which looks like a big leap in enthusiasm as it occurs, but the roots of this were set down five to ten years ago. I would say those roots included the final tipping point studies for senolytics, the spin-off of the SENS Research Foundation from the Methuselah Foundation, the injection of funding for SENS around then, and a number of other, related items.
It we look around today, a bigger community is planting a larger crop of seeds that will come to fruition in the mid-2020s, and today’s seeds include startup biotechnology companies in the SENS space, new advocacy initiatives like LEAF hitting their stride, and so forth.
Thanks to the efforts of many advocates, yours included, public perception of rejuvenation is also shifting. How close do you think we are to widespread acceptance?
I don’t think acceptance matters – that might be the wrong term to focus on here. Acceptance will occur when the therapies are in the clinic. People will use them, and everyone will conveniently forget all the objections voiced. The most important thing is not acceptance but rather material support for development of therapies. The help of only a tiny fraction of the population is needed to fund the necessary research to a point of self-sustained development, and that is the important thing. Create beneficial change, and people will accept it. Yet, you cannot just go and ask a few people. Persuading many people is necessary because that is the path to obtaining the material support of the necessary few: people do not donate their time and funds to unpopular or unknown causes; rather, they tend to follow their social groups.
Last year, you talked about the importance of sustained advocacy being as important as supporting the research itself. You wrote about a number of approaches to advocacy, including ours. Have you noticed an improvement in the quality of advocacy since then, and do you still maintain that professional advocacy is as important to the cause as research is?
Fishing for compliments? I’m very pleased with the progression of LEAF and with advocacy in general in our space. People have come and gone over the years, but this latest group of advocates appears to have set up shop for the long term. That is important and a welcome change. I can’t keep writing Fight Aging! forever, if only because hands and schedules eventually give way under the accumulated burdens of the years. There must be far more voices doing this same sort of work, all in their own varied ways. Diversity and redundancy are both important aspects of advocacy – many people arguing in their own ways for a given point of view are needed in order to persuade the world at large.
Presently, rejuvenation is a relatively unknown topic; people who say they’re against this technology probably don’t think it’s a concrete possibility anyway. However, as more important milestones will be reached—for example, robust mouse rejuvenation—this might change. Do you think that these milestones will result in opponents changing their attitudes or becoming more entrenched?
Opposition to human rejuvenation therapies is almost entirely irrational; either (a) it’s a dismissal of an unfamiliar topic based on the heuristic that 95% of unfamiliar topics turn out to be not worth the effort when investigated further, or (b) it’s a rejection of anything that might result in sizable change in personal opinion, life, and plans, such as the acceptance of aging and death that people have struggled to attain. This sort of opposition isn’t based on an engagement with facts, so I think a sizable proportion of these folk will keep on being irrational in the face of just any scientific advance or other new factual presentation short of their physicians prescribing rejuvenation therapies to treat one or more of their current symptoms of aging.
On the other hand, there will be steady progress in winning people over in the sense of supporting rejuvenation in the same sense as supporting cancer research: they know nothing much about the details, but they know that near everyone supports cancer research, and cancer is generally agreed to be a bad thing, so they go along. Achieving this change is a bootstrapping progress of persuading opinion makers and broadcasters, people who are nodes in the network of society. Here, milestones and facts are much more helpful.
After years of financially supporting other rejuvenation startups, you’re now launching your own company focused on gene therapies relevant to rejuvenation. What drove your decision to do this?
In the course of funding companies, one learns a great deal about the bounds of what might be achieved and the sort of work that is needed: it isn’t uncommon for investors to become entrepreneurs and vice versa. There are large overlaps in the mental toolkits required, and it is a logical evolution seen from either side. Moreover, in the course of investing in startups, one meets people in the community, such as my cofounder Bill, who intend to both fund and run companies, and it turns out that we work together quite well. As in all such things, it has a lot more to do with happenstance leading to the right arrangements of people and much less to do with the technical landscape at the time.
Your company’s first objective is thymic regeneration. Why do you think the thymus is the ideal initial target for your work?
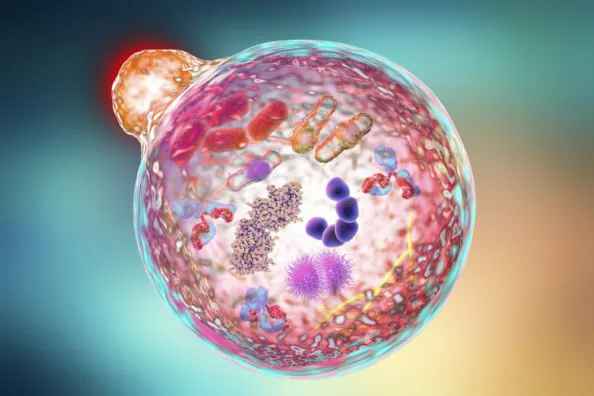
It is a very straightforward goal, with a lot of supporting evidence from the past few decades of research. It think it is important to set forth at the outset with something simple, direct, and focused, insofar as any biotechnology project can be said to have those attributes. This is a part of the SENS rejuvenation research agenda in the sense of cell atrophy: the core problem is loss of active thymic tissue, which leads to loss of T cell production and, consequently, immunodeficiency. However, the immune system is so core to the health of the individual that any form of restoration can beneficially affect a great many other systems. The many facets of the immune system don’t just kill off invading pathogens; they are also responsible for destroying problem cells (cancers, senescent cells), and they participate in tissue maintenance and function in many ways.
You are using gene therapy; why have you chosen this delivery method specifically and not, for example, a small-molecule approach?
If your aim is to raise or lower expression of a specific protein, and you don’t already have a small molecule that does pretty much what you want it to do without horrible side-effects, then you can pay $1-2M for a shot at finding a starting point in the standard drug discovery databases. That frequently doesn’t work, the odds of success are essentially unknown for any specific case, and the starting point then needs to be refined at further cost and odds of failure. This is, for example, the major sticking point for anyone wanting to build a small-molecule glucosepane breaker – the price of even starting to roll the dice is high, much larger than the funding any usual startup crew can obtain.
On the other hand, assuming you are working with a cell population that can be transduced by a gene therapy to a large enough degree to produce material effects, then $1-2M will fairly reliably get you all the way from the stage of two people in a room with an idea to the stage of having animal data sufficient enough to start the FDA approval process.
You are working with SRF spin-off company Ichor Therapeutics; what was the reason for choosing to work with Kelsey and the Ichor team?
Because they are great. Kelsey has achieved considerable success, bootstrapping from nothing but a plan, and has an excellent team. Their philosophy of development dovetails well with ours, both in terms of short-term development of a biotech startup and in the longer term of how we’d like to see this industry develop over the next 10-15 years.
Will your company focus on lab work, or do you plan to run human trials once a sufficiently advanced stage has been reached?
We’re absolutely signed up for the end-to-end path of getting a therapy into the clinic. That is the whole point of the exercise – to bring therapies into general availability. Of course, there will be a great deal of lab work to accomplish between here and there.
The FDA doesn’t recognize aging as a disease, so it won’t approve drugs to target it directly. Is this a problem for your company’s activities?
Remember that when talking to the FDA, one usually starts with just a small patient group with a single age-related condition, a fraction of everyone that might eventually be helped. This is done to control costs and ensure the best possible chance of a successful approval by narrowing the focus to a very clear, simple experiment. After this, one expands to larger patient groups and more expensive trials. As it happens, the effects of immunosenescence on health are so widespread and similar from individual to individual that it wouldn’t be hard to pick a clearly defined condition and patient population that covers near everyone in late life. Unfortunately, one would have to have very deep pockets indeed to pick that as the first option for entering the approval process – one has to work up to it.
What are Repair Biotechnologies’ possible future targets after thymic regeneration?
We’re looking into a couple of interesting options, guided by the SENS philosophy of damage repair, but it is very challenging to say at this stage which of them will prove the most advantageous to attempt. Obviously, at this stage, the primary focus has to be on success in our first venture.
What do you think are currently the most promising research avenues within each rejuvenation therapy subfield?
We have a challenge today in that we have the DNA of a patient advocacy community trying to get work to proceed at all. So, for fifteen years, our measure of success was “are people paying more attention to this?” Now, we have to start thinking like a development community, in which success revolves around “does this implementation actually work in humans, and how well does it work, and how much does it cost?”
In all too many cases, we don’t yet know the answers to these questions: the data isn’t there yet for senolytics, for example. So, you can look at senolytic efforts and know who has the most funding and attention but have no idea which of the therapeutic approaches actually represent the most significant progress at the end of the day. For all we know, dasatinib might turn out to be the most cost-effective of all of the current small-molecule approaches, with everything everyone has done since then coming in a poor second-best, and we won’t find this out for years, as no one has any incentive to run the necessary large-scale trials on an existing drug.
Dr. de Grey is hopeful, but not certain, that immunotherapy might make OncoSENS unnecessary. What do you think?
I have long thought that canonical OncoSENS – whole-body interdiction of lengthening of telomeres – might be rendered unnecessary by sufficiently advanced incremental progress in other areas of cancer research. That said, it should be so cost-effective that it is hard to imagine “sufficiently advanced incremental progress” not incorporating interference with telomeres in some way. People other than SENS-funded groups are working on it, after all.
If you think about it, restoring the immune system to youthful capacity should also help to achieve this goal; there is evidence to suggest that age-related immune dysfunction drives age-related cancer risk and that this correlates well with thymic decline. The world will still need highly effective, low-side-effect cancer therapies even if everyone has the cancer risk profile of a young adult, of course, but far less frequently.
What do you realistically expect might happen, over the next 25 years, in terms of rejuvenation research results, funding, clinical applications, and availability?
Well, that’s an essay in and of itself. I think my views on the technology itself are fairly widely known: I’ve written a few short essays on likely ordering of development. The funding will continue to grow year-over-year to the degree that any success is achieved in the clinic. However, everything takes a very long time in medicine due to the way in which regulation works, no matter how fast the technology is running in the labs, and the pace of technological progress in biotechnology is accelerating. At some point, the system exemplified by the FDA will break because cheap and effective therapies coming out of the labs will be so far ahead of what is available in the clinic that they will leak out into some other form of commercial development. Who knows what that will look like? Perhaps it will be a network of overseas non-profits that run their own, lighter and faster, validations of trials and presentations of human data gathered from participating clinics. I think that next-generation gene therapies, evolutions of CRISPR, will likely precipitate this sort of reordering of the landscape.
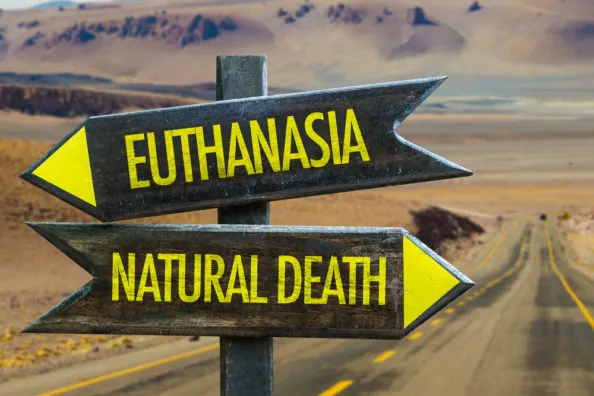
Do you expect that aging might relatively soon be officially considered a disease, or a co-morbid syndrome, by WHO and the FDA?
No. Regulation typically lags behind reality by many years. What will probably take place is some sort of battle of wills and lawyers over widespread off-label use for rejuvenation therapies, most likely senolytics, that have only been narrowly approved for specific age-related conditions. That will go on for a while and, ultimately, generate sufficient critical press attention to induce regulators to back off from trying to suppress that off-label use and, instead, accept aging as an approved indication. This hypothetical scenario could run a decade or more from beginning to end.
The availability of rejuvenation therapies doesn’t depend only on their cost; it also depends on how they’re regulated in each specific country. Do you imagine “rejuvenation tourism” will exist for long, or at all, before these treatments are part of the standard medical toolkit everywhere?
The development of stem cell therapies is the example to look at here. These therapies were available via medical tourism for a decade prior to the first approved treatments in the US, and this continues to be the case even afterwards, as only a narrow slice of therapies have been approved. Medical regulation is slow-moving, and so medical tourism will be long-lasting. I think this will work exactly the same way for other broad classes of therapy, such as gene therapies.
What is, in your view, the biggest bottleneck to progress in aging research?
Either (a) the lack of funding for research and early-stage startup development or (b) the low number of entrepreneurs, one of the two. Probably funding, as money can be used to craft an 80/20 solution to the shortage of entrepreneurs, but entrepreneurs can only reliably solve the lack of funding problem if there are a lot of them. Almost every specific instance of things not moving forward that I’ve seen could be addressed by a well-thought-out application of funds to the situation.
The chasm between academic research and early-stage commercial development is also a sizable issue. The academic side does a terrible job of reaching out to find entrepreneurs and companies that can carry forward their research to benefit patients. The entire biotechnology industry (entrepreneurs, investors, bigger companies and funding entities) collectively does a terrible job of reaching back into the academic community to fund, encourage, and adopt the most promising research. So, projects that should move instead languish for years because no one is taking the obvious steps to improve on the situation.
Right now, there don’t seem to be any unexpected problems with the science that might jeopardize the development of rejuvenation. Do you think that any particular areas of research might run into difficulties down the road?
No. I think all the unexpected problems will be implementation details. It is perfectly possible to have the correct strategy and the wrong tactics, and this happens all the time in complex fields such as biotechnology – it doesn’t take much of an error in interpreting research results to derail the original plan and require a new direction. Most such challenges are short-term and can be worked around with some loss of time and money, but there are certainly past instances in which the company is lost because there is no viable way to salvage a better path.
This is what happened to one of the early AGE-breaker efforts, the development of ALT-711: removing AGEs still seems very much a correct approach to the age-related stiffening of tissues, but a drug that works in rodents will do nothing in people because the physiologically relevant AGEs are completely different. At that time, the researchers didn’t have that critical piece of information. We will no doubt see similar stories occur again in the future.
Caloric restriction and exercise may also potentially convey some small increase in life expectancy. Given that the goal is to reach longevity escape velocity, do you practice a particular diet or exercise program, and would you encourage people to consider such approaches?
I have always suggested that people look into the simple, reliable things they can do for better health. The way to look at this is through the lens of cost-effectiveness. Calorie restriction and exercise are cheap, easy, and highly reliable. They don’t adjust your life expectancy by decades, but since they are cheap, easy, and reliable, you should still look into it. There are many different ways to approach both, so just because an attempt fails or isn’t palatable, that’s no excuse to give up on the whole endeavor. At the end of the day, it is a personal choice, of course. We can always choose to be less healthy; that’s easy to do in the present environment.
You’ve written many articles on the topic of self-experimentation on FA. Can you summarize your views?
The current self-experimentation community – and here I include many disparate groups, only tenuously linked, with interests in nootropics, anti-aging, muscle building, and so forth – is woefully disorganized and ill-educated when it comes to the risks and scientific knowledge of the compounds they try. If one in twenty of the people who have tried dasatinib as a senolytic have (a) read the papers on pharmacokinetics in human volunteers, (b) recalculated likely human doses from the senolytic animal studies and compared them with human chemotherapy studies, or (c) actually tested the compound delivered by a supplier to ensure purity, I would be astoundingly surprised.
The bar for quality and safety in this community needs to be raised, and that is the primary purpose behind my writing articles on self-experimentation. Whatever I say, people are going to be out there trying senolytics – many of these compounds are cheap, easily available, and hyped. What they should be doing instead of rushing in is thinking for themselves and reading widely. If I can do a little to help make that happen, then all to the good.
What is your take-home message for our readers?
There is always a way to help accelerate the development of rejuvenation therapies – there is always something that one can do and feel good enough about doing to do it well. Don’t know what that something might be? Then talk with people in the community. Reach out, go to meetings, post online. Don’t force it. It will come to you in time.
Best of luck to Reason and Bill in their new endeavor. If they can bring thymic rejuvenation to the clinic, they might possibly save millions of people from several devastating, age-related diseases.









 That being said, issues like inequity of resources, species extinction, and ecological destruction are legitimate concerns to be discussed and addressed, but their root lies chiefly in matters of policy, not population. A particularly salient example of this is the current situation in Venezuela, where its command and control economic structure has left the majority of the population
That being said, issues like inequity of resources, species extinction, and ecological destruction are legitimate concerns to be discussed and addressed, but their root lies chiefly in matters of policy, not population. A particularly salient example of this is the current situation in Venezuela, where its command and control economic structure has left the majority of the population Even if the power of the Infinity Gauntlet is somehow unable to solve the problem of limited resources directly, Thanos could surely use it to create a
Even if the power of the Infinity Gauntlet is somehow unable to solve the problem of limited resources directly, Thanos could surely use it to create a Perhaps if he were to be engaged on this directly, with earnest conversation rather than violent confrontation, he could come to see things differently.
Perhaps if he were to be engaged on this directly, with earnest conversation rather than violent confrontation, he could come to see things differently.