Today, we conclude our two-part interview with Dr. Michael Fossel, you can find part one here.
Changing tack a bit here, you talk a little bit in your book about programmed human death; we’re basically programmed to die through evolution’s weird workings and you kind of flesh out what Josh Mitteldorf calls the demographic theory of aging. Do you agree with that theoretic approach?
I think the teleology is wrong when we’re talking about programmed death. The usual programmed death meme goes something like this. I’m a great big tree, and I’ve got all these little trees that are growing underneath me; they’re my progeny, and I have to die to give them space to get to the sun. This becomes no longer science because I don’t know how you test this; to me, science is something you can test, and if you can’t test it, then stop calling it science; it becomes philosophy.
My argument would be that there are at least two levels of complexity going on here. One is that in any species, the shorter the lifespan, the faster the adaptation time. A lot of people tend to look at biology and ecology in a static sense, and they think that an organism has to adapt to its particular niche and the ecology, such as predators and prey. What they forget is that there’s no such niche and that the niche is always changing; if we have a long enough time span, the oxygen content of the atmosphere, the temperature of the Earth, and the acidity of the water all change dramatically over time, and they continue to change.
The same is true of an organism’s environment with regard to both its prey and its predators: the niche is always in flux. Niches are always changing. The first thing you would argue would be that you need the organism to be able to adapt fast enough to adapt to the rate of change in its niche. In bacteria’s case, you want something fast; human beings and elephants can take it more slowly.
The second thing I would argue, and that’s even more complex, is that you need to be able to adopt that rate of adaptation. For human beings, living for 75 years is fine if the environment isn’t changing very quickly. If the environment wasn’t changing [or changed very slowly], and we’re adapted to it, then we might be able to change the lifespan to adapt to that. In fact, that’s what you find if you look carefully. Again, I say this guardedly, because we’re not dealing with real data here, just a sort of correlational observation, but whenever you see a stressful situation in a [particular human] culture, what you see is that people tend to get married earlier and tend to die earlier. That makes sense, teleologically speaking; from an evolutionary perspective, that’s what should happen.
The lifespan of a species should adapt to the rate of change. The world around us is changing, but if the rate goes up or down, that has an effect on lifespan. If the world (or your niche) is changing slowly, then a long lifespan is evolutionarily desirable; if the world (or your niche) is changing quickly, then a short lifespan is absolutely necessary in order to keep up with that change and ensure the survival of the species. It’s remarkably complex.
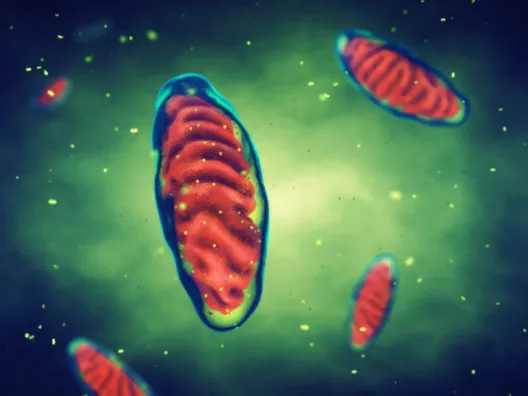
The other piece of this argument has to do with mutation rates. Most of us tend to think of mutations as bad. From your perspective, they are; from the species’ perspective, you can’t live without them. You’ve got to have a certain amount of rate of change. That means mutation. At any given moment, there’s an optimal rate of mutation for a species, but when you think about it, that’s not good enough. You need to be able to change that rate of mutation. So, if the environment’s changing, you need to change your mutation rate, not enough to kill your species but enough to increase the adaptation rate. When the telomeres shorten, the rate of mutation goes up.
So, as you get older, and as your telomeres shorten, your rate of mutation goes up; you’d expect that. If the environment changes fast enough, people are increasingly stressed, they are losing telomere length faster and they are dying young, which also means that they’re mutating faster. Not good for you, personally, but in general, we like to have that rate of mutation closely track the rate of environmental change. I think it does. This is not science; this is just observation and correlation, so I wouldn’t take it too seriously. It’s the best I can come up with.
So, then, you would agree that telomere shortening is very likely a programmed approach to ensure species health and ecosystem health?
Putting it simply, yes.
If we accept the programmed-death theory of aging, what does that tell us about the best way to mitigate aging?
Change the program.
And what’s the best way to do that?
As I’ve often said, I don’t actually care what causes aging, and I certainly don’t think telomeres cause aging. What I’d like to find is not what causes aging but what the single most effective point of intervention is, clinically and financially. From my perspective, that answer is telomeres and resetting both telomere length and gene expression.
If I want to deal with your heart disease, I can do a heart transplant. It’s expensive; it has side effects and risks. I can put in stents, I can do a coronary bypass graft, I can put you on statins. All of those things have an impact on your mortality from age-related vascular disease. I would argue that none of them are remarkable for being efficient clinically or financially.
What I’m looking for is the most effective intervention, clinically and financially. To me, the answer is telomeres. Not because they cause aging, but because it’s a handy place to reprogram what we just talked about as programmed aging.
A big concern here is that increasing telomerase activity may increase cancer risk. You discuss this in your book; you say pretty clearly your view is that, actually, given the data we have already from animal models and human studies, the more likely outcome from increased telomerase and thus longer telomeres is a mitigation of cancer risk. Can you flesh this out; do you still hold that view?
It’s actually a lot more complicated than that. Here’s the simplistic part that you just alluded to. First, let’s start with an observation. Whether you’re looking at mice with a lifespan of two years or humans with a lifespan of 80 years, if you plot out the incidence of cancer per unit of lifespan, the curves exactly overlap; you find an exponential increase in rate of cancer. You can almost pick your species, and it depends on whether the species is prone to cancer or not. For mice and humans, the exponential curves match. It’s two years and 80 years for the X axis, but it’s the same curve otherwise, just contracted.
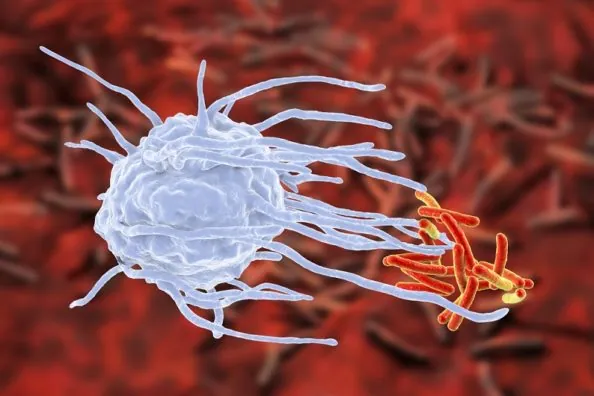
There are four major families of DNA repair enzymes, and every single one of them gets slowly turned down as cells become senescent and the gene expression changes. So, not only do you not identify the mutation in all of our cells, you don’t remove the abnormal base, replace the right base, and then ligate it into place. The rate of repair goes down, and that increases the likelihood of that mutation being passed on. That gets turned back up again when you reset gene expression.
The naive argument is that telomerase causes cancer. A slightly more sophisticated argument would be that telomerase prevents cancer, but the reality is more complex. It turns out that, in a simple analogy, we can look at two extremes. In one extreme, we’ve got a very young cell that has excellent DNA repair. It is not flawless, by the way. It’s just pretty darn good. So, you essentially have almost a zero rate of mutation. At the other extreme, you’ve got a senescent cell. The thing won’t divide no matter what you do; you can kick it as hard as you want, it won’t divide. It’s got all sorts of mutations and it’s still mutating, but it won’t divide, and so you don’t have cancer.
Except that, often, what happens is that those cells mutate just enough to express telomerase or use the ALT [Alternative Lengthening of Telomeres, a common way that cancer cells use to maintain telomere length] mechanism to extend telomere length just enough to permit cell division. So now, they’re still mutating all to hell, because they don’t have very long telomeres, but they’re just long enough to get another division and another division and another division. What you see is if you plot out telomere length versus rate of cancer and mutation, you find that with very long telomeres we see a low rate of mutation and a low rate of cancer. At very short telomere lengths, we see high rates of mutation and low rates of cancer. But, at pretty short but not completely short telomere lengths, you’ve got a huge peak where you’ve got a high mutation rate and the cells are still willing to divide. Bingo, you’ve got clinical cancer.
So, it’s not a simple curve. It’s two curves that overlap, and the peak point for cancer turns out to be pretty short telomeres but not completely short. If I take this back to a clinical case and say okay, that’s nice, but let’s get clinical here; let’s take a hundred patients, and let’s go ahead and treat them with telomerase, what’ll happen? It depends.
The quick answer is that you’d have a lower incidence of cancers coming on, and some of those cancers that they already have may be repaired, so you might be able to treat it, but not all. You’re going to have some cases where the mutation isn’t getting repaired; there’s still mutational damage in those cells, they’re still dividing, and they’ve got cancer. So, what is the outcome, clinically? The answer is that it’s complicated. Telomerase, in general, probably has benefits for cancer. That’s a nice blanket statement. But not for everything.
Let’s put a number around that. In terms of your confidence that telomerase therapy will actually mitigate cancer risk rather than increase it, what would you say the chances of that being true is, given your current state of knowledge of these mechanisms?
It’s not that simple, because, for some people, it’ll increase, for many people, it’ll decrease, so you’re looking at lumping all these people together. Let me put it in a different way, and this is a very practical way. Let’s say that I have Alzheimer’s disease, and you tell me that there’s an unknown, let’s say it’s 1 in 100, chance of increasing my cancer risk. Say it’s 1 in 10. Would I take it? The answer is “In a heartbeat,” because the Alzheimer’s is definitely going to kill me, and you’re telling me you’re not quite sure what the risk is, but it’s not zero.
Think of the practical outcome of this, which is another reason, in a strategic sense, we’re not going after wrinkles or osteoporosis. In all of human history, nobody’s died of osteoporosis, they’ve died of complications but not because of osteoporosis per se. With osteoporosis, you can break your hip and end up in the hospital, then you get pneumonia and die in the ICU. But, the osteoporosis didn’t kill you.
So, if I said I had an experimental treatment that may or may not cause cancer in a certain small percentage of people, we don’t know how much, would you take it for wrinkles? The answer is “Hell no, are you out of your mind?” For osteoporosis, the answer is “Come back in five years; tell me the results.” For cardiovascular disease, the answer is “I’ll think about it, but I have other options that may be as effective.” For Alzheimer’s, the answer is “Yes, absolutely.” That’s what I’m getting from the patients in our register, and that will be the most likely view from the FDA, too.
Do you see merit in the idea of “longevity escape velocity” (LEV)? This is the idea that initial therapies that address aging might add 10 years of extra lifespan, giving you enough time to benefit from the next improved versions of those therapies, which increases your lifespan further, and you keep on doing this.
Roughly. I’d add something else to it, which is that if I look back over the medicine of the past 200 years, we’ve made some interesting advances, and none of those advances involved things like robosurgery or wildly expensive new therapies. The things that had the greatest impact on human lives and suffering were hygiene when delivering babies, antiseptic surgery, germ theory, and vaccinations, which made a world of difference in terms of the medical stresses that you and I go through in our lives.
I think that we’re about to undergo something that will dwarf any of the medical changes that occurred in the last 200 years. We’re now finally, for the first time ever in history, going to be able to prevent and cure age-related diseases. Nothing we have done, ever, up until this point, has had any impact on the fundamental pathology of age-related diseases at all. We’ve all been treating symptoms. That’s about to change. We’re going to change not the mean lifespan, which has been going up for a while, but the maximum lifespan, which has never occurred.
The fact that we’re about to affect the maximum lifespan, to me, is interesting. I’m much more intrigued by the health and the suffering that play a role in people’s real lives.
Regarding senolytics (drugs that kill senescent cells), there have been some promising results from quercetin and dasatinib. Could you speak briefly about senolytics and about how people can experiment on themselves if they want to be very proactive?
I wouldn’t experiment with those, and I think that the approach is going to prove to be a problem. The rationale goes something like this. Say I’ve got a factory of a thousand people. In that factory, I notice that there are a hundred people who just don’t do their darn jobs. They’re just not very good at it, and I think that the thing to do is to fire them. Well, that’s okay, but that means that the other 900 people are going to have to do more work than before, and they’re going to grumble more. They’re going to have to work harder, they’re going to start complaining, and we’re going to have another hundred people who are now in the same position. If you keep firing the unhappy people and increasing the workload on the remainder, pretty soon you have an empty factory. What we’re advocating doing is not firing those hundred people [but instead] making them happy and effective workers.
Let’s take this down to the cellular level and look at your knee joint. Let’s say that ten percent of the cells are senescent. They’ve got SASP, gene expression that’s actually causing problems to neighboring cells. The senolytic approach is to remove those ten percent of the cells that are causing damage, and that sounds good, and, initially, it would be. The problem is that the remaining 90 percent have to divide to make up for the missing cells, which means that you’ve just accelerated senescence in the remaining cells. So, next year, you have to kill another 10 percent, and every time you do that, you’re increasing the rate of senescence of the remaining percentage of cells.
If you look at graphs of the published data, you find that, initially, there’s a little improvement in function, and then the vector goes down at a much steeper rate than when you don’t do anything at all. That’s what I think you’re going to find clinically. You’re going to find people with, for example, knee joints that have had senolytic therapy, and the osteoarthritis is gone for six months. Then, it starts creeping back, and next time you treat it, it comes back in five months, and then four months, and then it goes straight downhill and you get yourself an artificial joint. We’re suggesting that rather than temporary improvement followed by faster aging, the best approach is to reset the aging process itself by resetting gene expression. If you use telomerase gene therapy, you’ll end up with a young, functional joint. That’s the difference.
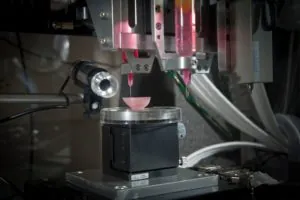
What about using iPS (induced pluripotent) stem cells to complement a senolytic approach to bring in new cells?
Kind of the same problem. It depends on where you get them. If you’re harvesting cells that have sufficiently long telomeres, then they’ll act like young cells. But, every time you do that, you have to go and spend the money to go through the process of getting those cells and hope that the cells are resetting telomere length completely, and most stem cells almost do, but they don’t, quite. So, over time, you’re still going to run into the same problem I just alluded to. The more iPS stem cells you harvest, the more senescent they will become.
The most effective approach is not to keep harvesting older and older cells but to reset cell aging and allow the younger, functional cells to cure the clinical problem. It’s a one-time treatment; you can come back in 10 years if you want and reset the clock again. You don’t need to keep adding (increasingly older) stem cells when you can instead simply reset the cells that are already in the tissue; the chondrocytes in the knee cartilage, for example, are perfectly capable of functioning if you just reset the telomeres. So, why waste time and money on iPS stem cells that are getting older with each treatment and are entirely unnecessary in the first place?
For the broader question of stem cell therapy, you’d say it’s easier to reset existing cells with telomerase therapy to be fully functioning than to transplant stem cells?
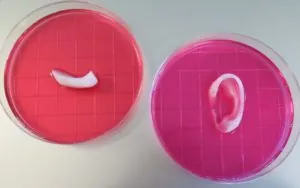
It depends. Let’s say you’ve got two knee joints, one of which has been replaced with an artificial joint and the other of which has bad osteoarthritis, and I say “Hey, I’ve got a wonder treatment; I’ve got telomere therapy, I can go fix the arthritic joint that’s still there,” and you go, “Great, thank you so much, what about my artificial joint?” Nope. My answer is that, once you’ve removed the natural joint, the only option is to use stem cells to rebuild the entire joint from scratch.
I can use telomerase gene therapy to cure a badly osteoarthritic joint, but once the joint has been removed, then you’ll need to use stem cells to rebuild it, although even then, you will want to use telomerase gene therapy to ensure that the stem cells are “young” and functional.
The point is that there are some things that telomerase therapy simply cannot do and will never be capable of doing. There are other things that stem cells can’t do and telomerase therapy can do. In that sense, there’s a complementarity there, but the complementarity isn’t simply a matter of using a little of both; it depends what you’re treating for.
There are companies claiming that they can predict, fairly reliably, the remaining years of life based on your epigenetic markers by using the Horvath clock. Is the data collected useful in terms of measuring aging?
About every three weeks, four weeks, I see another article come out that says something like “We took a hundred people and measured their telomere lengths. We instituted an intervention,” and here you can substitute diet, exercise, meditation, whatever. “We measured their telomere lengths six months later, and the telomere lengths were longer; therefore, we reversed aging.” Or, they say what you just said, which is “We measured a bunch of telomere lengths, and we tried to correlate with aging, and we think that we will predict it.” There are major problems with either of those types of papers. Almost all of the telomere lengths being measured are from leukocytes.
First, what is measured represents an extremely small percentage of the leukocytes around. So, it’s like saying, “I’m going to figure out what the average age of everyone living in New York is, so I’m going to measure the ages of 100 people working on one floor of one office building.” If the office building is in Manhattan, that’s not a good sample. The second problem is not even a technical one; it’s about how you measure because the wrong measure is mean telomere lengths rather than shortest telomere lengths. Then there’s the technical question of whether this measures the right cells. Your leukocytes divide peripherally. Let’s say the mean telomere length of a hematopoietic stem cell in the marrow is 10 kilo-base pairs. I don’t know that, because I didn’t do a bone marrow test on you. But I did a white cell sample on you, and I found that your mean telomere length was 9 kilo-base pairs [a very short telomere length]. But, at the same time, you just got fired from your job, your wife left you, your dog died, you have cancer and a virus, and you’re stressed. So, that’s part of why you have 9 kilo-base pairs.
But then, I Intervene and a few miracles occur: your wife comes back, your job is given back to you with a raise, you get over the viral infection, the cancer diagnosis turns out to have been an error, you buy a new dog, you’re fine, and you’re rich, and you’re happy. Now, what happens is you’re stressing your immune system less so that the churning of your white cells, peripherally, is going down, and now I measure your white cells and am getting 9.8 kilo-base pairs. I haven’t made you younger; all I’ve done is reduced the churning [of leukocytes].
This is like me saying there’s a block in Brooklyn that, 50 years ago, had a mean age of 73, and we’ve put in an urban renewal program, and it’s now got a mean age of 30. I haven’t made everybody younger; I’ve just changed the population I’m measuring. So, when you’re measuring your peripheral telomeres and predicting lifespan or measuring your methylation or your epigenetics, you’re measuring things that are peripheral and are churning, so you’d better measure them a lot over a number of years to get a good sample, otherwise, it’s not valid.
The other thing to remember is that if we are concerned about age-related disease, then peripheral leukocytes are the least of your problems. The majority of people on this planet are dying of vascular aging, which is to say endothelial aging, and I’ve never yet seen an article where somebody goes in, gets to snag a piece of your coronary artery, and measures telomeres in endothelial cells. Likewise, the second big group would be CNS sorts of dysfunctions, like Alzheimer’s. Nobody’s doing brain biopsy samples, I’m not surprised, nor would I want to do it or have it done to me. I wouldn’t do it to my patient.
However, even those studies that considered a gamut of human tissues are still missing the practical point, that of intervention. At its best, the Horvath clock is an overly complicated, data-intensive view of the outcome of telomere shortening. Far more importantly, the practical issue is the optimal point of intervention. As I’ve said before, we can’t reasonably address each and every one of thousands of genes and their percents of methylation using thousands of small molecular compounds, but we can use telomerase gene therapy to reset them all simultaneously and efficiently.
Could we develop a telomere clock?
We could if you focused on telomere loss rather than telomere length and if you focused on those cells that are clinically predictive for age-related disease, namely the endothelial cells of your arteries, the glial cells in your brain, the chondrocytes in your joints, etc. However, not only would this be ethically and technically difficult, but it’s not cost-effective either.
So, one, if you want to measure peripheral leukocytes, that’s okay, but you want to measure multiple times so you have time for all the various stresses in your life to even out. Two, that’s still not what kills you. If you’re one of those people who have very long telomeres, you’re a little more likely to have long telomeres not only in your leukocytes but in your CNS and elsewhere. If you’re one of those progeric kids who have short telomeres, yeah, you probably have them in your skin, your joints, and your endothelial cells. So, yeah, there is a correlation, but I’m not sure it’s worth paying money to get a study done.
In short, from a practical clinical perspective, I doubt the value of either a Horvath clock or a telomere clock. Let me put it this way: would you rather spend a lot of money to get information about some cell clock that may not be the best measure of your likelihood of getting a disease, or would you rather spend a lot less money to effectively cure and prevent age-related disease in the first place?
Thinking of future technologies, what do you think about the possibility of nanobots that can complete a comprehensive human bioassay relatively easily and cheaply?
I don’t know the value of that. It’s like saying, “Listen. I can do a genetics study, find out if you’ve got two ApoE4 alleles, which means that you have a slightly higher risk of getting Alzheimer’s disease. It will cost you $1000. Even if we know which alleles you have, that won’t improve your Alzheimer’s in any way. On the other hand, we could spend $10,000 and simply reset your genes and ensure that, whatever ApoE4 genes you have, we cure your Alzheimer’s disease.
What would you say? “Just cure it, I don’t care what my ApoE4 or ApoE2 is, I don’t really care.” I think that sooner or later, from a practical standpoint, that’s where we’re about to be with telomeres. In some sense, I don’t really care what my telomeres show, I just don’t want to die of an age-related disease, such as a heart attack or Alzheimer’s. Given a choice between finding out your risk (but not being able to prevent or cure the disease) or being able to prevent or cure the disease (but not measuring your telomeres or methylation), I think the human choice – and the medical choice – becomes quite clear. We want to improve health, not simply provide information about disease. Given a choice between academic measures of genes and methylation versus an effective treatment, I’ll take doing something, thank you.
Shifting gears, do you think that some real science is being done by “biohackers,” individuals experimenting on themselves?
There’s a long history of things like that, and the libertarian in me says “Go for it; you ought to just do it.”
On the other hand, as I said before, what I’m trying to do is cure Alzheimer’s on a worldwide basis, and I have to take a different approach because I have to convince other people, not myself, so it’s not a biohacker answer because nobody’s going to buy it, literally and figuratively.
So, in a generic way, I’m in favor of biohackers. One of the things I’ve always wanted to do is put together a crab apple tree that has luciferin and luciferase in it so that it’s bioluminescent and twinkles at night. I’ve always wanted to build that, but it’s probably illegal.
In light of everything you’ve said about telomerase therapy and gene therapy, it seems accurate to say that telomere therapy and most other kinds of rejuvenation therapies are various types of gene therapy. So, is the future of medicine in general gene therapy?
There are at least five different kinds of gene therapy. Some of them are things like CRISPR, where you’re rewriting the genes, some of them are things like what AveXis is doing, where they’re going and putting a new gene in, and some of this is things like designer bacteriophages to attack resistant bacteria. None of this has come to the clinic to my knowledge yet, although it’s very close in some cases.
Our telomerase therapy is a different approach from other gene therapies. Where we’re actually going is what I’ve been predicting for 50 years, which is that we’re going to end up with medicine divided into two categories: acute medicine (think trauma, poisonings, things like that) and gene therapy. Gene therapy will be used to fix things; acute medicine will be used for everything else. So, if you get hit by a truck, that’s acute medicine. If you have cancer, age-related diseases, or sickle cell, that’s gene therapy. Those are going to be the broad categories of medicine 50 years from now.
In Alzheimer’s research, there are two main camps, those who think tau protein is responsible for the disease and those who think that beta-amyloid is. In your book, you suggest that this is wrong and it is telomere attrition and the resulting gene expression changes that are the cause. Can you explain this a bit more?
Both tau protein and beta-amyloid are markers, not causes. Not surprisingly, when you treat markers instead of causes, you have almost no effect on the disease progression. It’s a bit like treating a patient in the ICU who has Ebola. Some people might notice they have a fever and want to treat that, and others see the patient has bleeding and try to treat that. That means you’re treating markers. What you need to do is kill the virus. You need to have an immune therapy or a vaccine for it. That’s what we’re dealing with here with Alzheimer’s. The wrong questions are: “Do I treat the fever?” and “Do I treat the bleeding?” for Ebola. The right question is: “Can you treat the underlying cause of these things?” In the case of Alzheimer’s, it’s not beta-amyloid, it’s not tau protein. Do they play a role? Yes. Are they pretty common in most of the patients? Absolutely. Do they actually cause damage? Absolutely, but they’re not the cause of the disease itself. The upstream cause has to do with changes in gene expression.
And why did you focus on Alzheimer’s? Is it more tractable than, say, cancer or heart disease, or do you think it’s equally intractable?
It’s a strategic reason that I alluded to earlier. One, it’s the high-hanging fruit. Everyone believes that Alzheimer’s can’t be cured, so if I do that, it’s a lot easier to go to step two, which is age-related vascular disease. The second reason has to do with the ethical and regulatory hurdles. As I said, if I’m treating osteoporosis, no one would be willing to undergo an experimental gene therapy at this point. On the other hand, if I’m treating Alzheimer’s, people are falling over themselves to volunteer for our trials. It’s strategic. Alzheimer’s disease is the “bogeyman” for most of us. We’re willing to do almost anything to cure it.
The other thing I’ve noticed is that if I go up to a thousand people and say, “How many of you have a neighbor, friend, relative, patient, or family member who’s got Alzheimer’s?” All hands go up. “How many of you don’t?” One hand goes up, and that one person is almost certainly very young, perhaps a teenager. When I talk about other things, people are not sure who’s got osteoporosis and who doesn’t. Everyone’s got wrinkles, and no one really cares, in a sense. Alzheimer’s is the bogeyman, so we’re going after it first. After that, vascular disease.
What do you see as the biggest challenge to a cheap and effective telomerase therapy?
That’s easy. It’s getting people to understand the model. I was talking with a chief scientist at a large, global pharmaceutical firm, a delightful woman, and the question was “Do you want to invest in us?” She said, “Where’s the evidence that telomerase therapy will lower beta-amyloid?” We said, “We don’t lower it, we just increase the turnover rate,” and I explain. In response, she said, “Okay, I get this, but where’s the evidence you’re lowering the total amount of beta-amyloid?” She doesn’t get it. She was still stuck in the static model in which beta-amyloid is a passive deposit that kills cells, and I couldn’t help thinking of the first car that pulled into a village in the middle of New England, the Model T, and an old man aks: “Where’s your horse?” The driver explains how the internal engine works, what gasoline does, and how the crankshaft turns the wheels. The old man listens politely, nods, and says, “Okay, I understand what you told me, and that’s fine, but I still have one question, which is: where’s the horse?”
And that’s what this chief scientist was doing. It’s not a question of a horse, it’s not a question of total beta-amyloid load, it’s a question of how fast it turns over. Getting that concept over to people is incredibly difficult.
They don’t get it. The people who get it most tend to be engineers because they’re used to what they call a systems approach. Biologists sometimes get it; the younger people get it. 20 years ago, if I asked what caused aging, I’d get these long explanations about reactive oxygen species and 40 other things. These days, I still get that from the 70-year-olds, but all of the young people, if they don’t know who I am, they’ve never heard of me, and I ask them to say what causes aging, the next five minutes will have the word “telomerase” or “telomere” in it, and we’ll talk about cell senescence. They don’t understand the model, but there’s a shifting acceptance that it plays a role someplace, which is fascinating to me. The biggest single problem is just that most people don’t get it. A few investors do, which is all I need right now.
You have seen the telomere theory of aging, for lack of a better term, kind of rise and fall in popularity and researchers supporting the notion. Is this dynamic mostly because of a lack of imagination or understanding?
Here’s another analogy. You and I, let’s say we’re back in the fifteenth century, and we’re in some little village in Eastern Europe, and you and I happen to know that smallpox will be devastating the village in a few months. It’s going to wipe out fully half of the village. We go to the local healers, and we explain how we can use cowpox vaccination to completely prevent smallpox deaths. The local healers, however, don’t understand what we’re telling them about viral infection and inoculation. The local healers have a different model, and they’re unwilling to re-examine their assumptions. The leading theory has to do with prayer, sin, demons, and the will of God, but nothing to do with viruses and the immune system. They don’t get it. They don’t see how vaccination can possibly affect what they see as the “real cause” of smallpox, which is original sin and God’s will.
To be fair, the local healers are truly knowledgeable about their herbs, and they have been effective for pain, fever, etc. But no matter what herbs they use, an herb really isn’t going to cure smallpox. The local healers are really good at herbal medicine, but they don’t get that smallpox is not a matter of willow bark and it’s not a matter of using foxglove. There’s something else going on, and the concept is very difficult to get through to people.
This is much the same problem that we have currently with Alzheimer’s disease. People start with assumptions about how these diseases work, their assumptions haven’t changed, and they don’t go back to look at the data and say “Let’s start again.”
What’s really going on here? The big pharma companies are beginning to realize that beta-amyloid just isn’t working out, but they’re having a hard time going back, re-examining all the assumptions, and asking, “Is there a better model, one that explains the disease accurately?” Too often, the answer is “Where’s the evidence it changes beta-amyloid?” The only thing to do is to fly the flying saucer down the National Mall and prove it. The hell with theories.
We would like to thank Michael for taking the time to talk to us about his work, and we wish him success in his attempt to defeat Alzheimer’s.