A collective of scientists has shown that osteoarthritis can be alleviated by guiding skeletal stem cells towards differentiation into chondrocytes, which are responsible for producing healthy cartilage [1].
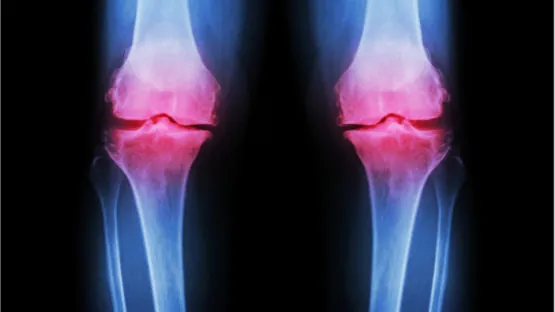
Osteoarthritis (OA) is a classic example of an age-related disease. While almost non-existent in younger people, it affects as much as half of the over-65 population worldwide. This is unsurprising given that OA is, basically, wear and tear: the degradation of joint cartilage as a result of lifelong friction and of age-related cellular dysfunction. Though OA by itself is not life-threatening, and the reports on its correlation with general mortality have been inconclusive [2], it can cause great discomfort or even disability, eroding the quality of life of people suffering from it. Defeating OA would be a major step towards increasing healthspan.
Since the 1950s, one of the popular OA treatments has been microfracture (MF) therapy, in which a minuscule injury is inflicted in the joint region, triggering tissue regeneration. This therapy is far from perfect since the regenerated tissue only vaguely resembles healthy cartilage. This “fibrotic cartilage” is essentially a type of scar tissue, as it contains a lot of fibrotic cells and has inferior mechanical properties. All MF can do is soothe OA symptoms to a degree.
MSCs or SSCs?
The mechanism behind MF therapy, as the authors of the current study have discovered, is the increased proliferation of skeletal stem cells (SSCs) triggered by microfracture. The term SSC is relatively new (or rather reintroduced) and requires a bit of explanation. Until recently, it was thought that stem cells that differentiate into bone and cartilage can be found not only in bone marrow but in other tissues as well, such as muscle and fat. These cells were named “mesenchymal stem cells” (MSCs), and this term is still widely used in the literature. However, more recent studies demonstrate that stem cells that differentiate into bone and cartilage exist exclusively in bone marrow, which is why some researchers insist that the term “skeletal stem cells” is more descriptive of the cells’ localization [3].
The researchers then set out to further elucidate the role that SSCs play in the regeneration of cartilage following MF. First, they tested the vitality of SSCs in relation to age. As expected, the prevalence of SSCs was found to be much lower in adult than in newborn mice. SSCs from adult mice also showed diminished proliferation ability, and when they differentiated into chondrocytes, they produced far fewer proteoglycans, the molecules that give cartilage its supreme weight-bearing abilities. Similar results were confirmed for human SSCs.
MF did more than just increase the proliferation of the local SSC population at the OA-affected joint. The transcriptional activity of genes in SSCs following MF was altered and became more reminiscent of the SSCs of young mice: MF reverted SSCs to a more juvenile type of gene expression.
Can this natural healing mechanism be further improved?
Previous studies have demonstrated that two key pathways, play an important role in tissue remodeling and homeostasis of cartilage [4]. One of these pathways, bone morphogenic protein 2 (BMP2), is known as a potent osteogenic growth factor. The other, vascular endothelial growth factor (VEGF), is normally a signaling protein that promotes the growth of new blood vessels. It drew the researchers’ attention because it had been shown that inhibiting VEGF signaling slows OA and fibrosis progression.
Separately, both factors produced disappointing results, but the simultaneous administration of BMP2 and inhibition of the VEGF pathway seemed to nudge SSCs towards differentiation into chondrocytes, which led to greatly increased cartilage formation.
Applying the cocktail to the MF site in a mouse OA model produced the desired effect. Together, BMP2 and VEGF inhibition stimulated robust formation of mostly normal, healthy cartilage (as opposed to the “fibrotic cartilage” produced by MF alone) and boosted proteoglycan production. Restoration of the biomechanical properties of the cartilage was further confirmed by improved mobility and gate of the treated mice.
MF-stimulated expansion of the SSC population was substantially slower in aged animals, which led to reduced cartilage regeneration. However, when MF-activated SSCs from young mice were transplanted to older mice undergoing MF-BMP2-VEGF therapy, they greatly contributed to stable cartilage formation.
Conclusion
By combining novel methods with this almost 70-year-old therapy, the researchers were able to overcome its limitations. For the first time, an intervention resulted in the formation of healthy cartilage at OA-affected sites. This achievement is hope-inspiring, given that OA remains a pressing and widespread problem that affects about half of the world’s elderly population. Since FDA-approved versions of BMP2 and VEGF signaling blockage are already in clinical use, this could potentially put a new groundbreaking OA therapy on the fast track for approval and deployment.
Literature
[1] Murphy, M. P., Koepke, L. S., Lopez, M. T., Tong, X., Ambrosi, T. H., Gulati, G. S., … & Steininger, H. (2020). Articular cartilage regeneration by activated skeletal stem cells. Nature Medicine, 1-10.
[2] Xing, D., Xu, Y., Liu, Q., Ke, Y., Wang, B., Li, Z., & Lin, J. (2016). Osteoarthritis and all-cause mortality in worldwide populations: grading the evidence from a meta-analysis. Scientific reports, 6(1), 1-7.
[3] Bianco, P., & Robey, P. G. (2015). Skeletal stem cells. Development, 142(6), 1023-1027.
[4] Ray, A., Singh, P. N. P., Sohaskey, M. L., Harland, R. M., & Bandyopadhyay, A. (2015). Precise spatial restriction of BMP signaling is essential for articular cartilage differentiation. Development, 142(6), 1169-1179.