Researchers are starting to test the use of immunotherapies, normally used for treating cancer, to target senescent cells, which accumulate in our bodies as we age and are implicated in many age-related conditions.
What are senescent cells?
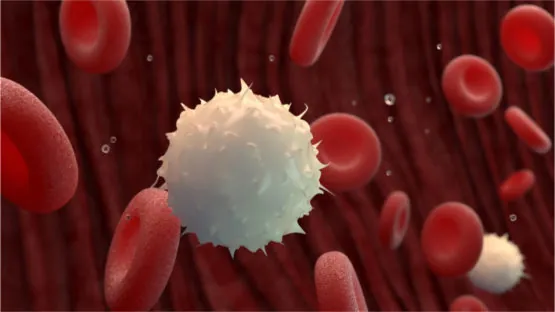
As you age, increasing numbers of your cells enter into a state known as senescence. Senescent cells do not divide or support the tissues of which they are part; instead, they emit a range of potentially harmful chemical signals that encourage nearby healthy cells to enter the same senescent state. Their presence causes many problems: they reduce tissue repair, increase chronic inflammation, and can even eventually raise the risk of cancer and other age-related diseases.
Senescent cells normally destroy themselves via a programmed process called apoptosis, and they are also removed by the immune system; however, the immune system weakens with age, and increasing numbers of senescent cells escape this process and begin to accumulate in all the tissues of the body.
By the time people reach old age, significant numbers of these senescent cells have built up, causing chronic inflammation and damage to surrounding cells and tissue. These senescent cells are a key process in the progression of aging.
One solution to the problem of senescent cell accumulation is to remove them using drugs or other therapies; such removal therapies are collectively known as senolytics.
Training the immune system to seek and destroy senescent cells
For decades, the foundation of cancer treatment has consisted of surgery, chemotherapy, radiation therapy, and targeted drug therapies. However, immunotherapies, which recruit and boost the power of a patient’s immune system to attack cancer cells, have risen to prominence to the point that many people in the cancer research community are calling them the “fifth pillar” of cancer treatment.
Chimeric antigen receptor (CAR-T) therapy is a type of immunotherapy that involves collecting a patient’s own immune cells, modifying them, and returning them to the patient to help fight a particular disease.
The backbone of CAR-T therapy are the T cells, the workhorses and soldiers of our immune system, which are primarily created in the thymus and trained in the lymph nodes. T cells play a central role in organizing our immune response and recruit other immune cells to help them destroy infected cells and invading pathogens.
During the CAR-T process, the collected T cells are genetically modified to produce receptors on their surfaces called chimeric antigen receptors (CARs). These receptors enable the T cells to identify and bind to a specific protein or antigen on target cells, usually tumor cells.
Once engineered to express the antigen-specific CAR, the collected T cells are then multiplied (expanded) in number, eventually reaching the hundreds of millions. The final step is then to reintroduce these supercharged immune cells back to the patient, where their newly engineered receptors help them to identify and destroy the target cells, which have the antigen on their surfaces.
While typically deployed against various cancers, the approach is now being explored for its utility against other diseases. The researchers of a new study have taken a CAR-T immunotherapy approach to removing senescent cells [1]. The team identified that urokinase-type plasminogen activator receptor (uPAR), a cell-surface protein, is widely activated in senescent cells and is a suitable target for CAR-T therapy to ablate the problematic senescent cells.
Cellular senescence is characterized by stable cell-cycle arrest and a secretory program that modulates the tissue microenvironment. Physiologically, senescence serves as a tumour-suppressive mechanism that prevents the expansion of premalignant cells and has a beneficial role in wound-healing responses. Pathologically, the aberrant accumulation of senescent cells generates an inflammatory milieu that leads to chronic tissue damage and contributes to diseases such as liver and lung fibrosis, atherosclerosis, diabetes and osteoarthritis. Accordingly, eliminating senescent cells from damaged tissues in mice ameliorates the symptoms of these pathologies and even promotes longevity. Here we test the therapeutic concept that chimeric antigen receptor (CAR) T cells that target senescent cells can be effective senolytic agents. We identify the urokinase-type plasminogen activator receptor (uPAR) as a cell-surface protein that is broadly induced during senescence and show that uPAR-specific CAR T cells efficiently ablate senescent cells in vitro and in vivo. CAR T cells that target uPAR extend the survival of mice with lung adenocarcinoma that are treated with a senescence-inducing combination of drugs, and restore tissue homeostasis in mice in which liver fibrosis is induced chemically or by diet. These results establish the therapeutic potential of senolytic CAR T cells for senescence-associated diseases.
Conclusion
The immune system is the ultimate living drug, and immunotherapies take that to the next level by making it stronger and better able to combat diseases. Using the same approach to address senescent cell accumulation and the myriad of age-related diseases that such accumulation facilitates is a logical next step for the technique.
This approach presents a viable alternative to searching for senolytic drugs, and if our own immune systems can be trained to go after unwanted senescent cells using common biomarkers present in senescent cell populations, our own cells become a senolytic therapy in their own right. In the not too-distant future, such a therapy combined with other immune system-boosting therapies and perhaps thymus rejuvenation could provide robust disease resistance in the elderly.