In a review paper, a group of scientists highlight a new strategy that addresses the shortcomings of stem cell therapy by adding T cell progenitors to the graft [1].
HSCT has a problem
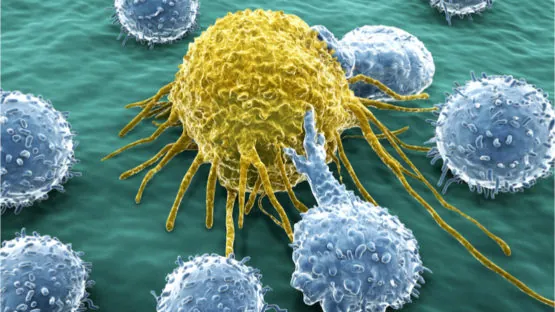
Today, one of the few ways to alleviate immune system damage from chemotherapy and radiotherapy is a hematopoietic stem cell transplant (HSCT), which is the only stem cell therapy in widespread use. This treatment, which has been around for over 30 years, aims to replenish the pool of HSCs, the common progenitors of immune cells, and to restore the host’s immune defenses. However, there is a problem: the T cell population recovers much more slowly than that of other populations. This discrepancy gets more noticeable with age: in older patients, the population may never fully recover. T cell deficiency hampers the anti-cancer response of the immune system regenerated by HSCT and leaves the patient vulnerable to pathogens. To mitigate this effect, many clinics add donor T cells to the graft (transplant), but because T cells are so aggressive, foreign T cells can induce graft vs. host disease (GvHD), a potentially deadly autoimmune attack on vital organs. To account for this danger, the patient is given immunosuppressants. Sadly, this balancing act usually fails, as most patients who receive HSCT succumb either to cancer relapse or to GvHD within five years after transplantation.
ProT instead of T
The authors of this new paper highlight a novel possible solution to this problem. Research has shown that transplanted HSCs fail to differentiate into T progenitor cells (ProTs). Therefore, the idea is to grow ProTs in vitro and add them to the graft, essentially bypassing the dysfunctional process of ProT production in the host. In recent research conducted by two of the authors of this paper, ProTs began to appear in the thymi of mice one week after transplantation [2]. After two weeks, the number of thymocytes grew significantly, suggesting successful proliferation of the donor ProTs. The transplantation also promoted the reconstitution of the thymus, apparently restoring the crosstalk between thymic epithelial cells and thymocytes. In other research, T cells derived from transplanted ProTs exhibited early anti-tumor activity, shortening the time during which the mice who received chemotherapy or radiotherapy remained immunocompromised.
A major advantage of ProTs compared to full-grown T cells is that the former lack T cell receptors (TCRs). TCRs are used by T cells to bind to cells in the body and destroy them. As a result, ProTs are unable to induce GvHD. Compatibility requirements can be less strict, as ProTs undergo the full process of selection and tolerization in the thymus anyway. T cells derived from transplanted ProTs show little to no autoreactivity.
T cells also exhibit strong heterogenity. Our body uses gene rearrangement to create a great variety of T cells with more than one billion different receptors that can recognize and counter virtually any pathogen. The researchers report that in preclinical mouse models, donor ProTs have been shown to successfully recreate this variety, enabling the host organism to combat both cancer and infections.
On a less positive note, ProTs cannot fully alleviate the age-related decline of our immune system. Although aged mice still benefit from ProT-enhanced HSCT, and the ProT engraftment in the thymus is successful in both young and old animals, ProTs proliferate up to ten times slower in the latter group. This shows how important it is to keep looking for ways to delay or reverse age-related thymic involution.
Conclusion
HSCT is the flagship of stem cell therapy. Unfortunately, its effectiveness is limited due to the autoreactivity of transplanted T cells and age-related thymic involution. By partially alleviating these problems, the strategy outlined in this new paper can potentially provide cancer patients with better and more immediate immune protection.
Literature
[1] Singh, J., Mohtashami, M., Anderson, G., & Zúñiga-Pflücker, J. C. (2020). Thymic engraftment by in vitro-derived progenitor T cells in young and aged mice. Frontiers in Immunology, 11, 1850.
[2] Singh, J., & Zúñiga-Pflücker, J. C. (2018). Producing proT cells to promote immunotherapies. International immunology, 30(12), 541-550.