In a study published in Cell Stem Cell, researchers have investigated a way to repopulate the brain with functional cells in order to fight back against Alzheimer’s disease.
A gene with a microglial function
Various allelles of the apolipoprotein E (APOE) genes are well-known for their contributions to, or defenses against, Alzheimer’s, as they affect how the brain processes the amyloids associated with the disease. However, that is not the only gene being explored. Here, the researchers focus on TREM2, a gene whose R47H variant has been identified as a strong risk factor for Alzheimer’s [1].
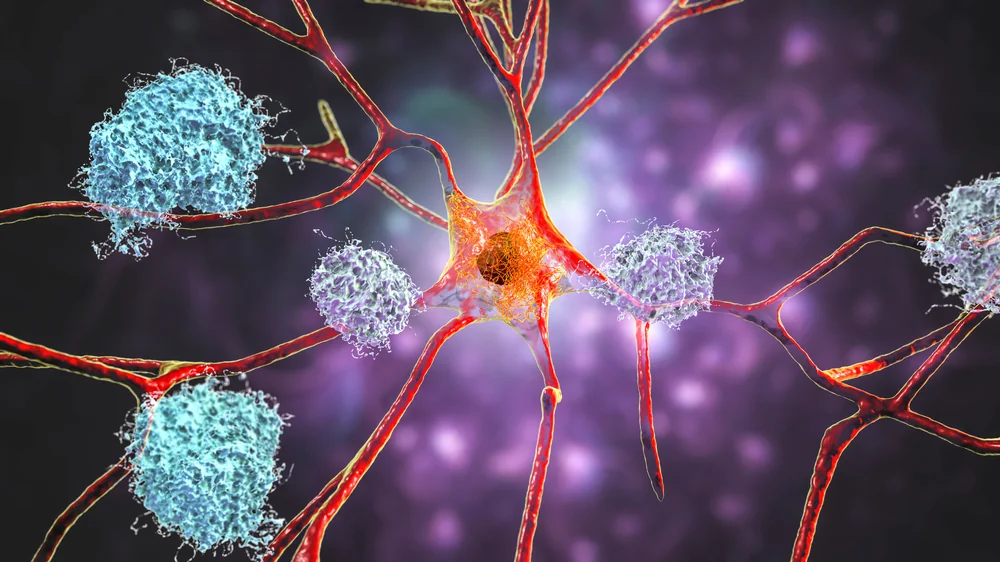
A complete loss of TREM2 is strongly associated with dysfunctional microglia, the cells that perform maintenance and immune functions in the brain. It results in Nasu-Hakola disease, a form of dementia that can cause bone cysts to form in the brain [2]. Other mutations of TREM2 can cause dementia even without bone cysts [3].
Since properly functioning TREM2 is so necessary for brain health, the researchers considered ways of restoring it to the brain. Rather than attempting to genetically modify cells in situ, they decided that introducing functional cells into the brain would be a more effective approach.
A process with doubly afflicted mice
Since mice do not naturally develop Alzheimer’s disease, genetically modified models are always required for studies. To proceed with this study, the researchers crossbred 5xFAD, a mouse model that exhibits Alzheimer’s at 6 weeks of age, with mice that express a reporter gene. The bone marrow of these mice was used in a technique called microglia replacement by bone marrow transplantation (mrBMT), which, true to its name, introduces circulation-derived myeloid cells (CDMCs) to serve the functions of microglia.
CDMCs are not the same as microglia, being smaller and more compact. However, the researchers found that they behave similarly towards amyloid beta plaques, wrapping tightly around them to prevent them from forming tendrils. CDMC-recipient mice and regular microglial mice had similar levels of amyloid beta load, which the researchers take as evidence that CDMCs are effective replacements for microglia in this model.
Next, the researchers used a doubly afflicted mouse model: mice that suffer from Alzheimer’s disease and are negative for the TREM2 gene. As expected, the microglia of these mice failed to respond properly to the amyloid plaques. CDMCs from other mice without TREM2, as expected, also failed to respond.
Effective on multiple levels
CDMCs from Alzheimer’s mice that did produce TREM2 were found to be effective. These transplanted cells rapidly wrapped around the amyloid plaques, slowing the spread of Alzheimer’s pathology within the brain, and were showing signs of phagocytosis: the attempt to engulf and consume these plaques. However, these cells were considerably more effective on 3-week-old mice than 8-week-old mice, suggesting that they are more effective when given early to suppress the disease.
Biomarkers of axonal damage, such as Lamp1, were also found to be relatively suppressed with this CDMC treatment. One biomarker of damage, the disease-associated microglia (DAM) program [4], was significantly upregulated; this represents the helper cells attempting to protect the brain. Signaling molecules and other effects of downstream gene expression was also found to be restored by CDMC treatment, including genes that handle the lipoproteins associated with brain function.
Potential for translational research
Obviously, this line of basic research is not going to directly lead to a cure for Alzheimer’s, especially in people without TREM2 deficiencies. However, it opens multiple avenues for translational research, the most obvious being that CDMCs may be effective in replacing microglia for this and other conditions. If the helper cells of the brain can be supplemented in ways that restrict the pathology of Alzheimer’s and other diseases, it might be possible to delay neurodegeneration and give people more healthy years of life.
Literature
[1] Jonsson, T., Stefansson, H., Steinberg, S., Jonsdottir, I., Jonsson, P. V., Snaedal, J., … & Stefansson, K. (2013). Variant of TREM2 associated with the risk of Alzheimer’s disease. New England Journal of Medicine, 368(2), 107-116.
[2] Paloneva, J., Autti, T., Raininko, R., Partanen, J., Salonen, O., Puranen, M., … & Haltia, M. (2001). CNS manifestations of Nasu–Hakola disease: a frontal dementia with bone cysts. Neurology, 56(11), 1552-1558.
[3] Chouery, E., Delague, V., Bergougnoux, A., Koussa, S., Serre, J. L., & Mégarbané, A. (2008). Mutations in TREM2 lead to pure early‐onset dementia without bone cysts. Human mutation, 29(9), E194-E204.
[4] Keren-Shaul, H., Spinrad, A., Weiner, A., Matcovitch-Natan, O., Dvir-Szternfeld, R., Ulland, T. K., … & Amit, I. (2017). A unique microglia type associated with restricting development of Alzheimer’s disease. Cell, 169(7), 1276-1290.