A study on animals with autoimmune myocarditis was recently released in the journal Cell Reports [1], showing the impact of heart inflammation on the types of immune cell that are formed in the heart. This could have a significant impact on our understanding of cardiac aging.
What is myocarditis and how is it relevant to aging?
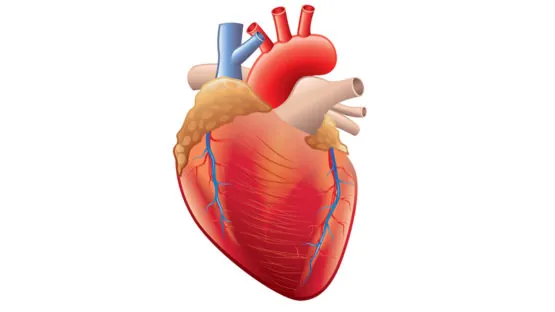
Myocarditis is a disease involving inflammation of the heart. It mainly influences people between the ages of 20 and 51 [2] [3]; however, the elderly are still affected to some degree. The disease has been known to cause serious complications, such as heart attack and heart failure.
Aging shares one similarity with myocarditis: inflammation. As myocarditis is caused by inflammation of the heart, studying it could tell us about how the heart changes with age due to constantly increasing age-related inflammation (inflammaging) [4].
An understanding of the changes that occur in the heart because of age-associated inflammation could allow the future creation of therapeutics that reverse these aspects of aging, which would lead to a decrease in heart attacks, strokes and heart failure in the elderly, thus improving health and lifespan.
What inflammation-associated changes are shown?
In the study, two mice had their circulatory systems connected, while one mouse had autoimmune myocarditis. The researchers showed significant changes in two different populations of immune cells (particularly monocytes and macrophages) along with changes in the local signalling environment because of this myocarditis.
One population – Ly6Chi monocytes, which are similar to human CD14+ monocytes and normally focused on clearance of harmful debris – were shown to create more inflammatory macrophages (immune cells with a variety of functions, including debris clearance and germ destruction) but were unable to clear the heart from harmful, inflammation-causing debris. While the rate of replication of this type of cell was unchanged, the rate of replication of another cell type was reduced, meaning that this inflammatory subtype became more common than other subtypes in the diseased heart.
This same population has been shown to cause fibrosis – scarring – of heart tissue in the diseased heart, which leads to the further creation of the same inflammatory macrophages in a positive feedback loop involving a signaling molecule (IL17A) that increases the number of these cells attracted to the diseased area through an intermediate molecule (CCL2) produced in scarred tissue, leading to further scarring and inflammation. These cells have also been shown to degrade the extracellular matrix (scaffolding) of the diseased heart, upon which its structure relies, and they possess proteins for recognizing certain germs, specifically class II antigen processing and presentation.
This same signaling molecule was also shown to cause scarred tissue to produce GM-CSF, a protein that encourages macrophages to mature into an inflammatory state (M1), despite the signaling molecule activating genes associated with a contradictory state as well (M2). Still, the behavior of the affected cells most matches the inflammatory subtype of macrophage, which has been shown to become more common in the body because of aging [5].
The increase in scarred heart tissue with an increase of the intermediate GM-CSF in the diseased heart has another impact – the prevention of the replication of Ly7Clo monocytes, which are most similar to CD16+ monocytes in humans – and the complete prevention of maturation of these cells into functional, scar-healing macrophages. As the diseased heart is a very hostile environment, this leads to the destruction of this subpopulation.
Of the cells that do mature in the diseased heart, unusually many of them originate from the very earliest, embryonic stages of life instead of being locally produced in the heart. This could be explained by the fact that the locally produced Ly6Clo cells have their replication and maturation systems shut down.
The overall macrophage population in the heart was shown to decrease, as could be expected because of the fact that Ly6Chi replication was not increased to compensate for the loss of the Ly6Clo cell population. In addition, the debris clearance-associated receptor MerTK on Ly6Chi monocytes and macrophages is prevented from being created, and is cleaved in the diseased heart, which could prevent clearance of harmful, inflammatory debris, accelerating the progression of the disease.
Conclusion
This study does have its weaknesses – since it is focused on mice, the same effects may not be seen in human cells. The merging of the circulatory systems of the healthy and diseased mice may be having some effect, and the disease itself may have other causes than the ones that aging has. Still, the trial gives some promising information that could inform further research.
Despite not being focused on a consequence of aging, myocarditis experiments like this could inform further research on an aged population. The next steps for research in this area should involve validation of the cell population changes, and, if the study is correct, methods to restore the initial balance of cell types.
Literature
[1] Hou, X., Chen, G., Bracamonte-Baran, W., Choi, H. S., Diny, N. L., Sung, J., … & Hackam, D. J. (2019). The Cardiac Microenvironment Instructs Divergent Monocyte Fates and Functions in Myocarditis. Cell reports, 28(1), 172-189.
[2] Kytö, V., Saukko, P., Lignitz, E., Schwesinger, G., Henn, V., Saraste, A., & Voipio-Pulkki, L. M. (2005). Diagnosis and presentation of fatal myocarditis. Human pathology, 36(9), 1003-1007.
[3]Fenoglio Jr, J. J., Ursell, P. C., Kellogg, C. F., Drusin, R. E., & Weiss, M. B. (1983). Diagnosis and classification of myocarditis by endomyocardial biopsy. New England Journal of Medicine, 308(1), 12-18.
[4] López-Otín, C., Blasco, M. A., Partridge, L., Serrano, M., & Kroemer, G. (2013). The hallmarks of aging. Cell, 153(6), 1194-1217.
[5] Becker, L., Nguyen, L., Gill, J., Kulkarni, S., Pasricha, P. J., & Habtezion, A. (2018). Age-dependent shift in macrophage polarisation causes inflammation-mediated degeneration of enteric nervous system. Gut, 67(5), 827-836.