Scientists have developed a protocol for hematopoietic stem cell transplantation that reconstructs a healthy blood system and prevents blood cancers in old mice while also reducing toxicity [1].
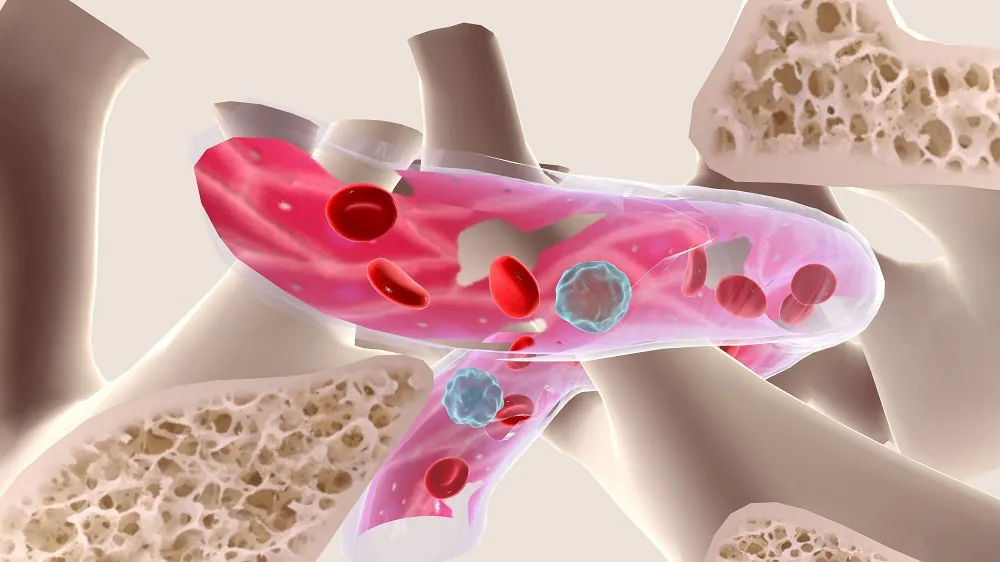
The blood factory
Hematopoietic stem cells (HSCs) work hard for our entire lives, producing vast numbers of various blood cells. As we age, this process, like many others in the body, gets dysregulated [2]. This contributes to the decline of the immune system and to the development of several harmful conditions, including blood cancers.
HSC transplantation is a feasible strategy, but it requires depleting the host’s own stem cells to make space in the bone marrow niche for the donor’s cells to engraft. Today, this is achieved mostly by chemo- and radiotherapies, which are notorious for their powerful side effects [3]. In a new study published in Nature Communications, researchers at the Lund Stem Cell Center at Lund University, Sweden, attempted to develop a safe and effective method for transplanting young, healthy HSCs into aged recipients.
“Conventional transplantation requires patients to undergo chemotherapy or irradiation to eliminate malignant cells, suppress immune rejection, and make room for new stem cells in the bone marrow,” explained David Bryder, Professor of Molecular Hematology at Lund University. “But these treatments are highly toxic, especially for older individuals, who are also the ones most likely to benefit.”
More cells, more drugs, less toxicity
First, the researchers tested an existing non-genotoxic conditioning agent, CD45-saporin (CD45-SAP), an immunotoxin that selectively eliminates HSCs without widespread toxicity, in both young (2-month-old) and aged (16-month-old) mice. Then, the team transplanted young HSCs and monitored the success of the transplant.
The team found that the conditioning was much less effective in aged mice. While CD45-SAP successfully depleted HSCs in young mice, a significant number of the host’s own HSCs remained in the aged mice. Consequently, when young HSCs were transplanted, they engrafted successfully and created new blood cells in the young mice but not in the aged group.
Having found that standard doses of HSCs fail to engraft well in aged mice, the researchers explored whether using a much larger number of donor HSCs could force a successful transplant. They expanded a small number of young HSCs into a large population ex vivo and then transplanted these cells into young mice, hypothesizing that the available niches for HSCs in the bone marrow might be more reliably populated if “flooded” with sufficient numbers of donor cells.
At this stage, the researchers used only young mice to prove that an increase in HSC numbers can improve transplantation outcomes. Transplanting large numbers of expanded HSCs indeed led to successful, long-term multilineage blood cell production even in unconditioned young hosts. Combined with CD45-SAP conditioning in young mice, the result was a robust and near-complete reconstitution of the blood system.
“In particular, the mice showed a strong resurgence in the production of naïve B and T lymphocytes, cells that play a key role in immune defense, which usually decline with age,” said Bryder. “These young cells didn’t just survive; they reshaped the entire immune landscape. We were especially encouraged to see that the new cells maintained long-term function and diversity, even within an aged environment.”
The researchers hypothesized that the primary problem with aged hosts was the failure to clear out enough of the old, resident HSCs. To fix this, they developed a more potent conditioning regimen by adding to the CD45-SAP immunotoxin a two-drug mobilization regimen (G-CSF/AMD3100), which forces the remaining host HSCs out of their protective bone marrow niches and into the bloodstream.
“Instead of using conventional chemotherapy, we deployed antibody-toxin conjugates, also known as immunotoxins, that selectively target and deplete the recipient’s own HSCs while sparing surrounding tissues,” explained Anna Konturek-Ciesla, postdoctoral researcher and first author of the study. “This was paired with a drug-based mobilization strategy that temporarily displaces stem cells from the bone marrow, creating space for incoming donor cells.”
Successful prevention in vivo
Finally, the researchers tested their strategy in a disease context, using a transgenic mouse model (NHD13) that is genetically predisposed to developing myelodysplastic syndrome (MDS) and acute leukemia, common blood disorders in elderly humans. They treated two-month-old mice with the combined conditioning regimen and transplanted healthy, wild-type bone marrow cells. The mice were then monitored for their entire lifespan.
In the untreated group, 75% of the mice developed blood malignancies, versus just 33% in the study group. Most strikingly, while 25% of untreated mice developed aggressive acute leukemia, none of the transplanted mice did.
The treatment was initiated at this young age because these transgenic mice develop symptoms early. The researchers also position their invention as “a prophylactic tool to delay or even prevent” the onset of age-associated hematological disorders. Potentially, non-toxic HSC transplantation can be used in an even wider context in order to prevent age-related immunosenescence, which is considered a major cause of aging and mortality.
“While these findings are currently limited to animal models, and there are many more steps to take before this can be applied in humans, they offer a proof-of-concept, that aged or malfunctioning stem cells can be safely replaced (without the toxicity of traditional conditioning) and that youthful blood production can be restored even in an older body,” summarized Konturek-Ciesla.
Literature
[1] Konturek-Ciesla, A., Zhang, Q., Kharazi, S., & Bryder, D. (2025). A non-genotoxic stem cell therapy boosts lymphopoiesis and averts age-related blood diseases in mice. Nature Communications, 16(1), 5129.
[2] Kim, M. J., Kim, M. H., Kim, S. A., & Chang, J. S. (2008). Age-related deterioration of hematopoietic stem cells. International journal of stem cells, 1(1), 55-63.
[3] Gyurkocza, B., & Sandmaier, B. M. (2014). Conditioning regimens for hematopoietic cell transplantation: one size does not fit all. Blood, The Journal of the American Society of Hematology, 124(3), 344-353.