After meeting him at the Astana Global Challenges Summit 2018, we’ve kindly been granted an interview by Dr. Anthony Atala, M.D., Director of the Wake Forest Institute for Regenerative Medicine and the W. Boyce Professor and Chair of Urology at Wake Forest University.
Dr. Atala is one of the most influential names in the field of regenerative medicine and biotechnology. His research focuses on growing human cells and tissues for use in transplants, and given the constant dire need for organ donors worldwide, his work is poised to improve—and save—the lives of millions. He and his team have already successfully engineered and transplanted bladders into living patients, and as he’s told us himself, more types of tissue have been engineered and tested in models; hopefully, they will one day be usable in patients as well.
Dr. Atala’s groundbreaking work has earned him countless awards, prizes, and nominations in well-known magazines, such as Scientific American, Time Magazine, the Huffington Post, and many others; he has also served on the boards and committees of several organizations, such as the National Institutes of Health, the National Cancer Institute, and SENS Research Foundation.
In addition to the aforementioned Global Challenges Summit, where he was part of a panel with Dr. Aubrey de Grey, Dr. Atala was one of the speakers at the Undoing Aging 2018 conference in Berlin, Germany, and we certainly hope to see him again during next year’s edition. Without further ado, here’s what Dr. Atala told us about regenerative medicine, tissue engineering, and aging. (All pictures in the interview below are courtesy of the Wake Forest Institute for Regenerative Medicine.)
What sparked your interest in regenerative medicine?
As a surgeon, I became interested in finding better solutions for patients who required repair with additional tissue, which was not available.
In 2009 and 2011, you gave very interesting TED talks about the state of tissue engineering and its potential to create replacement organs for transplants. At the time, transplantation of engineered bladders had already been successfully performed by your team, while kidneys were still a work in progress. How much has changed in the field since then?
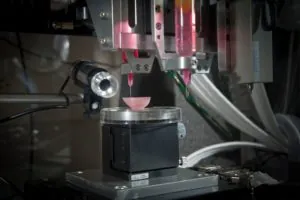
In addition to the bladder, Wake Forest Institute for Regenerative Medicine (WFIRM) scientists have successfully engineered several categories of tissues and organs and implanted them in patients. What has changed in this time period is the advancement of technologies with the creation of the Integrated Tissue and Organ Printing (ITOP) System, which was developed over a 12-year period by scientists at WFIRM.
We have printed bone, cartilage and muscle tissue that, when implanted in experimental models, developed a system of nerves and blood vessels. We showed that these structures have the correct size, strength and function for use in humans, proving the feasibility of printing living tissue structures to replace injured or diseased tissue in patients.
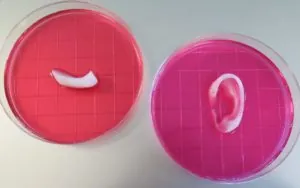
Ear and bone scaffold created by WFIRM’s Integrated Tissue-Organ Printing System in cell culture medium.
We are creating bioprinted organs like the kidney in the laboratory, but these are not yet ready for clinical use. The solid organs are the most challenging because they are dense with cells and have high oxygen requirements.
What’s the current situation in terms of need and availability of organs from human donors, and how much have engineered organs helped improve it so far?
We have successfully engineered several categories of tissues and organs and implanted them in small numbers of patients in clinical trials. These include flat organs such as skin, tubular organs such as urine tubes, and hollow, non-tubular organs such as the bladder. It is estimated that every 30 seconds, a patient dies from a disease that could be treated with tissue replacement, so the need is great.
Can we expect that tissue engineering will, one day, make organ donations completely unnecessary?

A bladder scaffold is “seeded” with cells and supports them as they grow and develop. Scaffolds are the essential components of tissue engineering efforts.
Someday in the future, regenerative medicine technologies may reduce the need for donors. There are simply not enough donor tissues and organs to meet demand, especially for kidneys. Regenerative medicine offers the hope of engineering replacement organs in the lab to help solve this shortage, and because these organs would be made with a patient’s own cells, there would be no issues with rejection.
Engineered organs may replace aged, failing organs as well as organs that fail for other reasons; however, do you think that cell therapies might allow us to repair existing organs rather than have to replace them?
We are working on many avenues of healing cell therapies for lung disease, diabetes, hemophilia and renal failure, for example. We have found that often the best strategy is to use the patient’s own tissue and organ-specific cells. We are pursuing multiple strategies to move our projects forward to meet our ultimate goal: making patients better.
The thymus starts shrinking at a very early age, eventually contributing to immunosenescence. How is progress going in creating a replacement thymus, and could the new organ carry on where the old one left off?
At WFIRM, we are working to apply tissue engineering techniques to create functional thymic tissue in order to fortify or replace the aging thymus, which has the potential to help restore the body’s immune response and ability to fight off infections.
One of the challenges of creating new organs is microvasculature; how are you overcoming the issues of ensuring that organs have ample blood vessel supply?
Vascularization is indeed a challenge for the most complex tissues, such as solid organs. We are using a number of strategies to help overcome these challenges, including bioprinting.
It is said that the heart is one of the most challenging organs to create; why is this so, and how is progress in engineering new hearts going?
The solid organs like the heart are the most complex to engineer. These are the most challenging because they are dense with cells and have high oxygen requirements. We have engineered solid organs that are not fully functional in vitro.
What is the major challenge when engineering new organs for a patient?
Vascularization for tissues and organs continues to be an area of research focus. The Integrated Tissue and Organ Printing (ITOP) System allows for a lattice of micro-channels to be printed throughout the structure in order to allow nutrients and oxygen from the body to diffuse and keep them alive while the tissues develop their own system of blood vessels and integrate with the body.
Is there a “holy grail” of regenerative medicine—for example, a particular kind of tissue that is still not possible to engineer?
Engineering fully functional solid organs, such as the kidney, liver and heart, is considered the “holy grail” of the regenerative medicine field.
Barring the effects of substance abuse and similar factors, do all our organs fail more or less at a similar rate, or are some of them especially long-lasting compared to others?
A person’s vital organs begin to lose some function as they age during adulthood, and aging changes occur at all levels in the body’s systems. Aging is a complex process and includes many influences, such as heredity, environment and diet, that affect an organ’s rate of failure. There is no way to predict exactly how anyone will age.
Albeit far more popular than it used to be, the idea of using regenerative medicine to extend healthy lifespan, possibly by a considerable amount, is still somewhat controversial in that many people still don’t approve of it. What do you think of it?
Our approach to regenerative medicine is to improve people’s lives. The intent is not to prolong lives, necessarily, but to ease suffering. For example, someone experiencing kidney failure will someday, hopefully, be able to have a new implanted kidney made from their own cells, which means no rejection nor any need for anti-rejection medicines for the rest of their lives.
Scientists studying the biology of aging or the applications of regenerative medicine to aging, such as Dr. David Gems and Dr. Aubrey de Grey, seem to agree that intervening directly on the root causes of aging might dramatically extend both healthspan and lifespan. Are you equally optimistic that this might be the case?
I believe that in the process of providing a solution for failing tissues and organs, one is, in fact, prolonging that patient’s lifespan. This definitely makes sense. We still have much to learn about aging, but it is inspiring to know that so much progress has been made in just the last decade.
I am definitely optimistic about the continued progress in the field of aging. New approaches are being developed, and new therapies are now evolving.
What is the biggest bottleneck to progress in tissue engineering?
We need to advance regenerative medicine manufacturing, like Henry Ford did with the automobile assembly line. Last year, WFIRM announced the launch of a five-year, $20 million effort involving a public-private partnership that involves the U.S. Army Medical Research and Materiel Command and the Medical Technology Enterprise Consortium (MTEC). This partnership has the goal of improving the manufacturing process to hopefully speed up the availability of replacement tissues and organs for patients.
Do you have a take-home message for our readers?
Not so long ago, the field of regenerative medicine was considered science fiction, and now so much of it has become fact. It is an exciting field that has the power to heal and improve patients’ lives, which is our ultimate goal.
We would like to thank Dr. Atala for this interview, and we share his excitement and hopes for the future of tissue engineering and its potential to revolutionize the way we do medicine. If, as he says, facts of today were science fiction in the recent past, there are good chances that the promises of today’s pioneering sciences may be the norm in the near future.