Low-Dose Naltrexone: Benefits and Side Effects
Naltrexone is a medication approved by the FDA to treat opioid addiction and alcohol dependence. This drug was developed in 1961 [1-2].
Naltrexone blocks the action of opioids at three key receptors that regulate a range of bodily functions. These include immune function, cell growth and proliferation, and mood and cognition. Naltrexone was typically given in doses ranging from 50 to 150 milligrams per day. This is enough to continuously block these receptors.
In the late 1980s, Dr. Bernard Bihari noted that his patients with AIDS had low endorphin levels. He knew that raising natural endorphin levels could help the immune system. Dr. Bihari thought that briefly blocking opioid receptors might increase natural endogenous opioids [3-4].
He started giving low dose naltrexone (LDN) to his AIDS patients. He noticed their natural opioids increased and their immune function improved. Since then, LDN has been prescribed to treat immune system dysregulation, neurotransmitter depletion, and, in some cases, cancer.
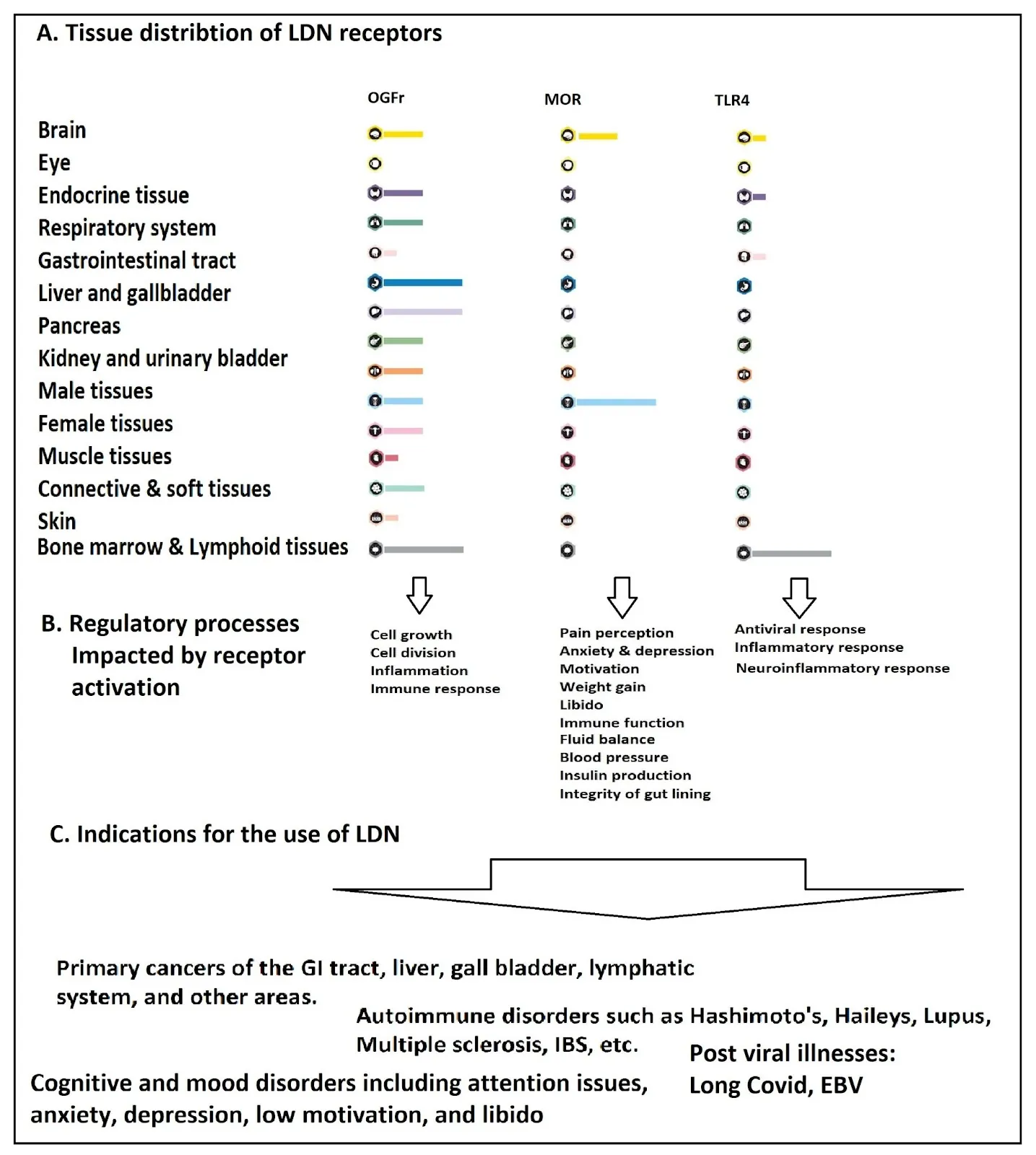
Low-dose naltrexone works by temporarily blocking certain receptors [5-6]. These include the opioid growth factor receptor (OGFr), Toll-like receptor 4 (TLR4), and the Mu opioid receptor (MOR).
The location of these receptors and how they signal help explain the use of LDN. It also suggests its potential as a longevity drug.
OGFr and opioid growth factor (OGF)
OGFr expression is highest in monocytes, microglia, and lymphocyte immune cells. Cells from the reproductive and urinary systems, digestive organs, digestive tract, adrenal glands, and breast tissue have OGFr. However, these tissues have about ten times less OGFr than immune cells.
Certain cells of the nervous system also express significant amounts of OGFr. These include cells from the prefrontal and cerebral cortex, the spinal cord, and the retina [7].
OGF is normally engulfed by cells in a process called clathrin-mediated endocytosis [8]. Once inside the cell, it attaches to OGFr located on the surface of the cellular nucleus, forming a complex. The OGF-OGFr complex is then guided into the nucleus, where it binds to DNA and stimulates the production of p16INK4a and p21 [9-10].
These two proteins, in turn, slow down cell division. In addition, p16INK4a inhibits the action of NFkB, a central player in initiating the inflammatory response [11].
When LDN is given, it temporarily blocks the OGFr receptor. This leads to an increase in the number of OGFr receptors and OGF. As LDN blockage wears off in the following hours, the effects of OGF and OGFr are amplified.
This leads to less cell growth and fewer cells multiplying [10]. The inflammatory response also goes down [12]. This effect helps control cell growth, promotes healing, reduces inflammation, supports immune function, and boosts autophagy [13-17].
LDN can slow down cell growth and division. This suggests it may help treat cancers in tissues with high OGFr expression. This includes primary cancers of organs like the bladder, testis, ovaries, breast, lung, lymph nodes, adrenal glands, and bone [18]. LDN can affect cancer development through OGFr, but this is not the only way it might prevent cancer.
The effect of LDN on immune cell growth may explain how it affects patients with multiple sclerosis. LDN reduces the growth of CD4+ and CD8+ T cells. It also affects B220+ lymphocytes found in the spleens and lymph nodes of multiple sclerosis patients.
This effect may also occur in other conditions in which the immune system is overactive [19]. People with autoimmune diseases often have low levels of opioids [20].
Toll-like receptor 4 (TLR4)
TLR4 is activated by patterns of molecules found on the surface of pathogens. Thus, it is referred to as a pattern recognition receptor.
When TLR4 is activated, NFkB, AP1, and IRK3 are also activated as part of the downstream signaling cascade. AP1 functions similarly to NFkB. IRK3 specifically triggers the production and release of interferon 1, which initiates the antiviral response.
In a healthy body, these three signaling molecules help manage the response to infection. Unfortunately, in autoimmune disease, this triad of signaling molecules can become hyperactive, resulting in chronic inflammation.
TLR4 expression is highest in immune cells, including monocytes, microglia, and peripheral blood mononuclear cells. TLR4 acts as a detector for pathogens. So, it is most concentrated in parts of the body that are at risk of infections. These include the reproductive and urinary system, the liver, and the heart.
The reproductive organs are vulnerable to sexually transmitted diseases. The liver is also vulnerable. It constantly gets foreign debris from the digestive system and spleen through the hepatic portal circulation.
The heart cannot handle damage from heart injury or infections. These can happen easily in people with bad oral health and other conditions [21]. Patients with heart failure frequently have elevated levels of TLR4 expression [22].
LDN temporarily blocks TLR4 signaling. This means it could potentially reduce inflammation and antiviral responses in certain tissues. However, it seems that blocking TLR4 temporarily does not lead to an increase in TLR4 receptors. This is different from what happens with opioid receptors.
If TLR4 increased as a response, LDN would boost TLR4 signaling. This would raise inflammation and drive the antiviral response. Blocking TLR4 seems to strengthen the anti-inflammatory effects of blocking OGFr in the immune system. It does this by reducing cytokine production.
Evidence suggests that low-dose naltrexone may help the viral immune response in people with chronic IFN-1 activity. [23]. This suggests that LDN may help treat post-viral syndromes. These include Epstein-Barr, chronic fatigue syndrome, and long COVID.
Taken together, these results suggest that transient blocking of TLR4’s signaling cascade can temporarily reduce the immune response. So, using LDN could help treat autoimmune diseases. Itt may work even better due to its effect on OGFr activity.
Microglia, the nervous system’s version of macrophages, are activated when PAMPs bind to TLR4. Overactivation of microglia can lead to inflammation, pain sensitivity, fatigue [24], sleeplessness [25], mood disorders, and cognitive problems [24,26]. When microglia are chronically activated, as they are with fibromyalgia and other pain disorders, it results in neurotoxicity. Thus, LDN may improve outcomes in several neurodegenerative diseases.
Mu opioid receptor (MOR)
LDN has a strong affinity for the Mu opioid receptor (MOR) [27]. Like OGFr, transient MOR blockage results in increased production of opioid receptors and enhanced sensitivity to opioids [28]. MOR receptors are distributed throughout the central and peripheral nervous systems as well as the skin [29-31]. Evidence indicates that the binding of LDN to MOR primarily affects pain perception and dopamine secretion [32].
The graphic below provides a summary of LDN receptors by tissue type.
LDN and pain management
Opioid receptor blockage causes a compensatory increase in opioid receptors [28]. This increases opioid receptor sensitivity to any concentration of opioids. However, opioid binding to GABAergic brain cells prevents the release of GABA, which, in turn, stops pain signals.
Some evidence suggests that LDN does not exert its reported effects on pain reduction in this manner. This is despite what would appear to be strong theoretical underpinnings for it to do so [33].
LDN and dopamine
A similar mechanism would lead to an increase in dopamine secretion. In this case, stopping GABA release increases dopamine release. This change can bring many benefits since low dopamine symptoms are well-known.
These include chronic pain, anxiety, and depression [34]. They also include attention difficulties, low motivation, and constipation [34]. Other issues are weight gain [35], trouble swallowing [36], and sleep disorders [37]. Fatigue [38], low libido [39], and a generally poor mood are also common [40].
Most dopamine is produced in one of two places: the adrenal glands and the hypothalamus. Adrenal dopamine has numerous functions and is released as part of the fight-or-flight reaction [41].
It relaxes blood vessels at low doses and helps remove excess sodium and urine from the body [42]. It reduces insulin production [43], protects the GI lining [44], and reduces lymphocyte activity in the immune system [45].
Dopamine originating in the hypothalamus is strongly associated with the brain’s reward system. When individuals engage in activities associated with survival, the brain releases dopamine, which induces a sense of pleasure. This provides the motivation to repeat the behavior. This also explains in part how exogenous opiates can lead to addiction [46].
LDN works on MOR and can help reduce pain, anxiety, and depression. It may also improve attention, motivation, and weight control. Additionally, it could enhance sleep, libido, and energy levels.
LDN may also help improve conditions like IBS, Crohn’s disease, and other gut disorders. This is due to its effects through OGFr.
LDN and weight loss
Contrave is a prescription drug approved by the FDA. It combines 8 milligrams of naltrexone with 90 milligrams of bupropion. Naltrexone is released slowly, while bupropion is an extended-release antidepressant.
Contrave is for obese people with a BMI of 30 or higher. It is also for those with a BMI of 27 or higher who have high cholesterol or controlled high blood pressure [47].
The proposed way that Contrave helps with weight loss is by using bupropion. Bupropion boosts the release of a hormone called aMSH, which reduces appetite.
However, bupropion also induces the secretion of endogenous opioid products that inhibit aMSH. Naltrexone is thought to solve this problem. It does this by blocking the effects of opioid products on aMSH [48-49].
An 8-milligram extended-release dose of naltrexone would not be considered LDN. Evidence supporting LDN for weight loss is limited; however, there is reason to believe that LDN could support weight loss.
There is evidence that increasing endogenous endorphin levels can improve insulin control [50]. Better insulin control has many benefits. These include easier fat loss, lower disease risk, fewer cravings, improved brain health, and better cognition [51].
Additionally, chronic inflammation is associated with metabolic syndrome and weight gain. Therefore, the anti-inflammatory effects of LDN could support weight loss [52]. There is limited evidence to support this theory.
LDN may indirectly stimulate increases in fat-burning growth hormone, as insulin is a growth hormone antagonist. Naltrexone has been shown to reduce insulin output in some contexts [53-54]. Finally, LDN may improve sleep, and poor sleep is associated with weight gain [55].
Wilfrid Noel Raby, PhD, MD, is an adjunct clinical professor at Albert Einstein College of Medicine. He prescribes very low-dose naltrexone at night to help with insomnia. He explains that stopping the cortisol surge in the evening lowers sympathetic activity. This helps people fall asleep faster.
LDN works quickly and causes a rise in cortisol in the morning. This helps with alertness during the day and to improve sleep at night [56].
It is important to note that LDN can cause sleep problems when you first start taking it. This effect usually does not last long [57].
Can LDN increase longevity?
LDN is likely to influence several hallmarks of aging. Aging is known to drive chronic inflammation, a condition known as inflammaging. Rising numbers of senescent cells, the accumulation of advanced glycation end-products, and other age-related changes drive inflammaging. LDN has shown the potential to mitigate inflammaging through multiple routes.
The binding of LDN to OGFr suppresses NFkB, AP1, and IRK3, all of which are inflammatory compounds. Additionally, LDN’s binding to the TLR4 complex short-circuits inflammation. It also may potentially block the binding of glycated LDL and other AGEs that harm aging tissues through TLR4 [58].
LDN can slightly boost natural opioids in the body. This suggests it may help reduce stress and improve well-being. Stress has been shown to drive telomere shortening, one of the reasons we age [59]. It is likely there are other potential mechanisms through which LDN could affect the hallmarks of aging as well.
Low-dose naltrexone side effects
Evidence supports the safety and tolerability of LDN in the treatment of multiple sclerosis, fibromyalgia, and Crohn’s disease. Subjective reports indicate that patients experience reduced pain and improved quality of life. However, studies documenting the objective benefits of LDN in these diseases are limited [60].
The most reported side effects for LDN are transient sleep disturbance and mild headache [57]. Sleep disturbance, usually in the form of vivid dreams, occurs in about 37% of patients. A small minority also experience nightmares [61].
Some physicians have anecdotally reported anxiety and tachycardia as adverse reactions to LDN. Reports of this nature are sprinkled across the internet. As anxiety is a known symptom of opioid withdrawal. This means it’s possible that some individuals would experience anxiety due to blockade of endogenous opioids.
Interestingly, naltrexone has also been reported as a treatment for orthostatic tachycardia, and endorphins, in general, reduce anxiety [2,62].
Literature
[1] W. W. Shen, “Anticraving therapy for alcohol use disorder: A clinical review,” Neuropsychopharmacol. reports, vol. 38, no. 3, pp. 105–116, Sep. 2018, doi: https://doi.org/10.1002/npr2.12028
[2] A. B. Srivastava and M. S. Gold, “Naltrexone: A History and Future Directions,” Cerebrum, vol. 2018, p. cer-13-18, Sep. 2018, [Online]. Available: https://pubmed.ncbi.nlm.nih.gov/30746025
[3] B. Bihari, “Bernard Bihari, MD: low-dose naltrexone for normalizing immune system function,” Altern Ther Heal. Med., vol. 19, no. 2, pp. 56–65, 2013.
[4] B. Bihari et al., “LOW DOSE NALTREXONE IN THE TREATMENT OF ACQUIRED IMMUNE DEFICIENCY SYNDROME,” in IV International AIDS Conference, 1988, no. June, pp. 1–12.
[5] D. Singh and A. Saadabadi, “Naltrexone,” StatPearls [Internet], pp. 1–3, Feb. 2022, Accessed: Apr. 03, 2022. [Online]. Available: https://www.ncbi.nlm.nih.gov/books/NBK534811/
[6] T. K. Eisenstein, “The Role of Opioid Receptors in Immune System Function ,” Frontiers in Immunology , vol. 10. 2019, [Online]. Available: https://www.frontiersin.org/article/10.3389/fimmu.2019.02904
[7] U. Mathias et al., “Tissue-based map of the human proteome,” Science (80-. )., vol. 347, no. 6220, p. 1260419, Jan. 2015, doi: https://doi.org/10.1126/science.1260419
[8] F. Cheng, P. J. McLaughlin, W. A. Banks, and I. S. Zagon, “Internalization of the opioid growth factor, [Met5]-enkephalin, is dependent on clathrin-mediated endocytosis for downregulation of cell proliferation,” Am. J. Physiol. Integr. Comp. Physiol., vol. 299, no. 3, pp. R774–R785, Jun. 2010, doi: https://doi.org/10.1152/ajpregu.00318.2010
[9] I. S. Zagon, M. F. Verderame, and P. J. McLaughlin, “The biology of the opioid growth factor receptor (OGFr),” Brain Res. Rev., vol. 38, no. 3, pp. 351–376, 2002, doi: https://doi.org/10.1016/S0165-0173(01)00160-6
[10] R. N. Donahue, P. J. McLaughlin, and I. S. Zagon, “Low-dose naltrexone targets the opioid growth factor–opioid growth factor receptor pathway to inhibit cell proliferation: mechanistic evidence from a tissue culture model,” Exp. Biol. Med., vol. 236, no. 9, pp. 1036–1050, Sep. 2011, doi: https://doi.org/10.1258/ebm.2011.011121
[11] P. Ghiorzo et al., “Inverse correlation between p16INK4A expression and NF-?B activation in melanoma progression,” Hum. Pathol., vol. 35, no. 8, pp. 1029–1037, 2004, doi: https://doi.org/10.1016/j.humpath.2004.02.017
[12] R. N. Donahue, P. J. McLaughlin, and I. S. Zagon, “The opioid growth factor (OGF) and low dose naltrexone (LDN) suppress human ovarian cancer progression in mice,” Gynecol. Oncol., vol. 122, no. 2, pp. 382–388, Aug. 2011, doi: https://doi.org/10.1016/j.ygyno.2011.04.009
[13] P. J. McLaughlin, J. D. Cain, M. B. Titunick, J. W. Sassani, and I. S. Zagon, “Topical Naltrexone Is a Safe and Effective Alternative to Standard Treatment of Diabetic Wounds,” Adv. wound care, vol. 6, no. 9, pp. 279–288, Sep. 2017, doi: https://doi.org/10.1089/wound.2016.0725
[14] M. R. K. L. Lie et al., “Low dose Naltrexone for induction of remission in inflammatory bowel disease patients,” J. Transl. Med., vol. 16, no. 1, pp. 1–11, 2018, doi: https://doi.org/10.1186/s12967-018-1427-5
[15] D. K. Patten, B. G. Schultz, and D. J. Berlau, “The Safety and Efficacy of Low-Dose Naltrexone in the Management of Chronic Pain and Inflammation in Multiple Sclerosis, Fibromyalgia, Crohn’s Disease, and Other,” Pharmacother. J. Hum. Pharmacol. Drug Ther., vol. 38, no. 3, pp. 382–389, Mar. 2018, doi: https://doi.org/10.1002/phar.2086
[16] Z. Li, Y. You, N. Griffin, J. Feng, and F. Shan, “Low-dose naltrexone (LDN): A promising treatment in immune-related diseases and cancer therapy,” Int. Immunopharmacol., vol. 61, pp. 178–184, 2018, doi: https://doi.org/10.1016/j.intimp.2018.05.020
[17] L. Cao, M. Fu, S. Kumar, and A. Kumar, “Methamphetamine potentiates HIV-1 gp120-mediated autophagy via Beclin-1 and Atg5/7 as a pro-survival response in astrocytes,” Cell Death Dis., vol. 7, no. 10, pp. e2425–e2425, 2016, doi: https://doi.org/10.1038/cddis.2016.317
[18] D. R. Couto and J. D. B. Fernandes, “Low Doses Naltrexone: The Potential Benefit Effects for its Use in Patients with Cancer,” Current Drug Research Reviews, vol. 13, no. 2. pp. 86–89, 2021, doi: https://dx.doi.org/10.2174/2589977513666210127094222
[19] P. J. McLaughlin, D. P. McHugh, M. J. Magister, and I. S. Zagon, “Endogenous opioid inhibition of proliferation of T and B cell subpopulations in response to immunization for experimental autoimmune encephalomyelitis,” BMC Immunol., vol. 16, p. 24, Apr. 2015, doi: https://doi.org/10.1186/s12865-015-0093-0
[20] M. D. Ludwig, I. S. Zagon, and P. J. McLaughlin, “Serum [Met5]-enkephalin levels are reduced in multiple sclerosis and restored by low-dose naltrexone,” Exp. Biol. Med., vol. 242, no. 15, pp. 1524–1533, Aug. 2017, doi: https://doi.org/10.1177/1535370217724791
[21] R. A. Seymour, P. M. Preshaw, and J. G. Steele, “Oral Health and Heart Disease,” Prim. Dent. Care, vol. os9, no. 4, pp. 125–130, Oct. 2002, doi: https://doi.org/10.1308/135576102322481947
[22] P. B. Katare, P. K. Bagul, A. K. Dinda, and S. K. Banerjee, “Toll-Like Receptor 4 Inhibition Improves Oxidative Stress and Mitochondrial Health in Isoproterenol-Induced Cardiac Hypertrophy in Rats,” Frontiers in Immunology, vol. 8. 2017, [Online]. Available: https://www.frontiersin.org/article/10.3389/fimmu.2017.00719
[23] A. Murira and A. Lamarre, “Type-I Interferon Responses: From Friend to Foe in the Battle against Chronic Viral Infection,” Frontiers in Immunology, vol. 7. 2016, [Online]. Available: https://www.frontiersin.org/article/10.3389/fimmu.2016.00609
[24] T. Singhal et al., “Regional microglial activation in the substantia nigra is linked with fatigue in MS,” Neurol. – Neuroimmunol. Neuroinflammation, vol. 7, no. 5, p. e854, Sep. 2020, doi: https://doi.org/10.1212/NXI.0000000000000854
[25] M. Bellesi, L. de Vivo, M. Chini, F. Gilli, G. Tononi, and C. Cirelli, “Sleep Loss Promotes Astrocytic Phagocytosis and Microglial Activation in Mouse Cerebral Cortex,” J. Neurosci., vol. 37, no. 21, pp. 5263–5273, May 2017, doi: https://doi.org/10.1523/JNEUROSCI.3981-16.2017
[26] X. Wang et al., “Pharmacological characterization of the opioid inactive isomers (+)-naltrexone and (+)-naloxone as antagonists of toll-like receptor 4,” Br. J. Pharmacol., vol. 173, no. 5, pp. 856–869, Mar. 2016, doi: https://doi.org/10.1111/bph.13394
[27] P. Mannelli, Peindl, and L.-T. Wu, “Pharmacological enhancement of naltrexone treatment for opioid dependence: a review,” Subst. Abuse Rehabil., p. 113, 2011, doi: https://doi.org/10.2147/sar.s15853
[28] H. M. B. Lesscher, A. Bailey, J. P. H. Burbach, J. M. Van Ree, I. Kitchen, and M. A. F. M. Gerrits, “Receptor-selective changes in µ-, δ- and κ-opioid receptors after chronic naltrexone treatment in mice,” Eur. J. Neurosci., vol. 17, no. 5, pp. 1006–1012, 2003, doi: https://doi.org/10.1046/j.1460-9568.2003.02502.x
[29] S. Ständer, M. Gunzer, D. Metze, T. Luger, and M. Steinhoff, “Localization of µ-opioid receptor 1A on sensory nerve fibers in human skin,” Regul. Pept., vol. 110, no. 1, pp. 75–83, 2002, doi: https://doi.org/10.1016/S0167-0115(02)00159-3
[30] K. Gach, A. Wyrebska, J. Fichna, and A. Janecka, “The role of morphine in regulation of cancer cell growth,” Naunyn. Schmiedebergs. Arch. Pharmacol., vol. 384, no. 3, pp. 221–230, Sep. 2011, doi: https://doi.org/10.1007/s00210-011-0672-4
[31] C. Stein, M. Schäfer, and A. H. S. Hassan, “Peripheral opioid receptors,” Ann. Med., vol. 27, no. 2, pp. 219–221, 1995, doi: https://doi.org/10.3109/07853899509031962
[32] Z. Z. Pan, “µ-Opposing actions of the κ-opioid receptor,” Trends Pharmacol. Sci., vol. 19, no. 3, pp. 94–98, 1998, doi: https://doi.org/10.1016/S0165-6147(98)01169-9
[33] M. J. Metz, C. M. Daimon, and S. T. Hentges, “Reported benefits of low-dose naltrexone appear to be independent of the endogenous opioid system involving proopiomelanocortin neurons and ß-endorphin,” eNeuro, vol. 8, no. 3, pp. 1–11, 2021, doi: https://doi.org/10.1523/ENEURO.0087-21.2021
[34] G. J. Sanger, “Chronic constipation: improved understanding offers a new therapeutic approach,” J. Physiol., vol. 594, no. 15, pp. 4085–4087, Aug. 2016, doi: https://doi.org/10.1113/JP272560
[35] J. Reinholz, O. Skopp, C. Breitenstein, I. Bohr, H. Winterhoff, and S. Knecht, “Compensatory weight gain due to dopaminergic hypofunction: new evidence and own incidental observations,” Nutr. Metab. (Lond)., vol. 5, p. 35, Dec. 2008, doi: https://doi.org/10.1186/1743-7075-5-35
[36] S. Polychronis, G. Dervenoulas, T. Yousaf, F. Niccolini, G. Pagano, and M. Politis, “Dysphagia is associated with presynaptic dopaminergic dysfunction and greater non-motor symptom burden in early drug-naïve Parkinson’s patients,” PLoS One, vol. 14, no. 7, pp. e0214352–e0214352, Jul. 2019, doi: https://doi.org/10.1371/journal.pone.0214352
[37] K. Dzirasa et al., “Dopaminergic control of sleep-wake states,” J. Neurosci., vol. 26, no. 41, pp. 10577–10589, 2006, doi: https://doi.org/10.1523/JNEUROSCI.1767-06.2006
[38] E. Dobryakova, H. M. Genova, J. DeLuca, and G. R. Wylie, “The dopamine imbalance hypothesis of fatigue in multiple sclerosis and other neurological disorders,” Front. Neurol., vol. 6, p. 52, Mar. 2015, doi: https://doi.org/10.3389/fneur.2015.00052
[39] J. A. Cocores, N. S. Miller, A. C. Pottash, and M. S. Gold, “Sexual Dysfunction in Abusers of Cocaine and Alcohol,” Am. J. Drug Alcohol Abuse, vol. 14, no. 2, pp. 169–173, Jan. 1988, doi: https://doi.org/10.3109/00952999809001544
[40] J. M. Jarcho, E. A. Mayer, Z. K. Jiang, N. A. Feier, and E. D. London, “Pain, affective symptoms, and cognitive deficits in patients with cerebral dopamine dysfunction,” Pain, vol. 153, no. 4, pp. 744–754, 2012, doi: https://doi.org/10.1016/j.pain.2012.01.002
[41] S. R. Snider and O. Kuchel, “Dopamine: An Important Neurohormone of the Sympathoadrenal System. Significance of Increased Peripheral Dopamine Release for the Human Stress Response and Hypertension*,” Endocr. Rev., vol. 4, no. 3, pp. 291–309, Jul. 1983, doi: https://doi.org/10.1210/edrv-4-3-291
[42] M.-Z. Zhang et al., “Intrarenal dopamine deficiency leads to hypertension and decreased longevity in mice,” J. Clin. Invest., vol. 121, no. 7, pp. 2845–2854, Jul. 2011, doi: https://doi.org/10.1172/JCI57324
[43] D. Aslanoglou et al., “Dopamine regulates pancreatic glucagon and insulin secretion via adrenergic and dopaminergic receptors,” Transl. Psychiatry, vol. 11, no. 1, p. 59, 2021, doi: https://doi.org/10.1038/s41398-020-01171-z
[44] G. Eisenhofer et al., “Substantial Production of Dopamine in the Human Gastrointestinal Tract,” J. Clin. Endocrinol. Metab., vol. 82, no. 11, pp. 3864–3871, Nov. 1997, doi: https://doi.org/10.1210/jcem.82.11.4339
[45] C. Strell et al., “Divergent effects of norepinephrine, dopamine and substance P on the activation, differentiation and effector functions of human cytotoxic T lymphocytes,” BMC Immunol., vol. 10, no. 1, p. 62, 2009, doi: https://doi.org/10.1186/1471-2172-10-62
[46] G. Di Chiara and V. Bassareo, “Reward system and addiction: what dopamine does and doesn’t do,” Curr. Opin. Pharmacol., vol. 7, no. 1, pp. 69–76, 2007, doi: https://doi.org/10.1016/j.coph.2006.11.003
[47] Orexigen Therapeutics, “CONTRAVE Package Insert Revised 9/2014 (naltrexone HCl and bupropion HCL) Extended-Release Tablets.” La Jolla, CA.
[48] T. Ornellas and B. Chavez, “Naltrexone SR/Bupropion SR (Contrave): A New Approach to Weight Loss in Obese Adults,” P T, vol. 36, no. 5, pp. 255–262, May 2011, [Online]. Available: https://pubmed.ncbi.nlm.nih.gov/21785538
[49] R. Plodkowski, N. Quang, S. Umasankari, L. Nguyen, D. Chau, and S. St Jeor, “Bupropion and naltrexone: a review of their use individually and in combination for the treatment of obesity,” Expert Opin. Pharmacother, vol. 10, no. 6, pp. 1069–1081, 2009.
[50] C. F. Su, Y. Y. Chang, H. H. Pai, I. M. Liu, C. Y. Lo, and J. T. Cheng, “Infusion of ß-endorphin improves insulin resistance in fructose-fed rats,” Horm. Metab. Res., vol. 36, no. 8, pp. 571–577, 2004, doi: https://doi.org/10.1055/s-2004-825763
[51] L. Clamp, D. Hume, E. Lambert, and J. Kroff, “Enhanced insulin sensitivity in successful, long-term weight loss maintainers compared with matched controls with no weight loss history,” Nutr. Diabetes, vol. 7, no. e282, 2017.
[52] D. P. Cardinali and R. Hardeland, “Inflammaging, Metabolic Syndrome and Melatonin: A Call for Treatment Studies,” Neuroendocrinology, vol. 104, no. 4, pp. 382–397, 2017, doi: https://doi.org/10.1159/000446543
[53] L. De Marinis et al., “Influence of chronic Naltrexone treatment on growth hormone and insulin secretion in obese subjects,” Int. J. Obes., vol. 21, no. 11, pp. 1076–1081, 1997, doi: https://doi.org/10.1038/sj.ijo.0800519
[54] A. Choubey et al., “Low-dose naltrexone rescues inflammation and insulin resistance associated with hyperinsulinemia,” J. Biol. Chem., vol. 295, no. 48, pp. 16359–16369, Nov. 2020, doi: https://doi.org/10.1074/jbc.RA120.013484
[55] S. R. Patel and F. B. Hu, “Short Sleep Duration and Weight Gain: A Systematic Review,” Obesity, vol. 16, no. 3, pp. 643–653, Mar. 2008, doi: https://doi.org/10.1038/oby.2007.118
[56] B. Yasgur, “Common Bedfellows: Sleep Disturbances and Psychiatric Disorders – Psychiatry Advisor,” Psychiatry Advisor, 2020. (accessed Apr. 07, 2022).
[57] K. Toljan and B. Vrooman, “Low-Dose Naltrexone (LDN)—Review of Therapeutic Utilization,” Med. Sci., vol. 6, no. 4, p. 82, 2018, doi: https://doi.org/10.3390/medsci6040082
[58] C. P. Hodgkinson, R. C. Laxton, K. Patel, and S. Ye, “Advanced Glycation End-Product of Low Density Lipoprotein Activates the Toll-Like 4 Receptor Pathway Implications for Diabetic Atherosclerosis,” Arterioscler. Thromb. Vasc. Biol., vol. 28, no. 12, pp. 2275–2281, Dec. 2008, doi: https://doi.org/10.1161/ATVBAHA.108.175992
[59] J. K. Kiecolt-Glaser and R. Glaser, “Psychological stress, telomeres, and telomerase,” Brain. Behav. Immun., vol. 24, no. 4, pp. 529–530, May 2010, doi: https://doi.org/10.1016/j.bbi.2010.02.002
[60] D. K. Patten, B. G. Schultz, and D. J. Berlau, “The Safety and Efficacy of Low-Dose Naltrexone in the Management of Chronic Pain and Inflammation in Multiple Sclerosis, Fibromyalgia, Crohn’s Disease, and Other Chronic Pain Disorders,” Pharmacother. J. Hum. Pharmacol. Drug Ther., vol. 38, no. 3, pp. 382–389, Mar. 2018, doi: https://doi.org/10.1002/phar.2086
[61] J. Younger, L. Parkitny, and D. McLain, “The use of low-dose naltrexone (LDN) as a novel anti-inflammatory treatment for chronic pain,” Clin. Rheumatol., vol. 33, no. 4, pp. 451–459, 2014, doi: https://doi.org/10.1007/s10067-014-2517-2
[62] L. B. Weinstock, J. B. Brook, T. L. Myers, and B. Goodman, “Successful treatment of postural orthostatic tachycardia and mast cell activation syndromes using naltrexone, immunoglobulin and antibiotic treatment,” BMJ Case Rep., vol. 2018, 2018, doi: https://doi.org/10.1136/BCR-2017-221405

