The newest study published in the International Journal of Molecular Sciences investigates the role senescent cells may play in cerebral ischemia-reperfusion injury and how senolytic therapy may be beneficial for those recovering from stroke.
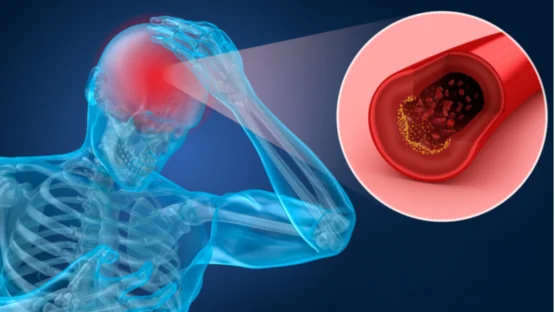
Stroke and reperfusion injury
Ischemic stroke occurs when an artery in the brain is occluded, preventing an area of brain tissue from receiving fresh oxygen and nutrients from the bloodstream. It is one of the leading causes of death and disability and occurs primarily in elderly individuals [1].
Timely treatments can restore blood flow to the ischemic tissue and reduce the severity of the stroke. While restoring blood flow is critical to the tissue’s survival, reperfusion itself has been shown to set off a cascade of events, contributing to the overall tissue damage [2]. Referred to as ischemia-reperfusion (IR) injury, this damage-causing cascade involves inflammation and reactive oxygen species (ROS) [3].
Read More
Cellular senescence is a state that is pro-inflammatory and anti-proliferative. Because of its connection to aging, the cellular stress response, ROS, and inflammation, researchers at Seoul National University hypothesized that it may play an important role in IR injury. They tested this hypothesis in both in vitro and in vivo models. Additionally, they investigated whether the senolytic drug ABT263 (Navitoclax), which selectively kills senescent cells, could alleviate some of the effects of IR injury [4].
IR induces senescence in astrocytes, which can be eliminated by ABT263 in vitro
In cell culture, IR injury was modeled by first depriving rat astrocytes of oxygen and glucose, then reintroducing both into the culture system. This process did not cause cell death, but SA-ß-gal staining (a measure of senescence) increased from 22% to 60% of cells.
These cells were then treated with ABT263. After treatment, cell viability remained unchanged in astrocytes that were not exposed to the IR injury model. The ones that were, however, had their viability decrease. SA-ß-gal positive cells also decreased from 60% to 36% of the population.
ABT263 alleviates IR injury in rats
IR injury in vivo was modeled by occluding and re-opening the middle cerebral artery in rats. This occlusion was associated with an increase in the expression of senescence marker p16 and the inflammatory markers NOS2 (also a SASP factor), MPO, and GFAP. Meanwhile, ABT263 treatment reduced their expression to non-IR injury levels. Treatment also reduced the infarct volume by more than half and improved behavioral measures of neurological function.
In conclusion, this study demonstrated that intravenous ABT263 treatment attenuated inflammation through elimination of senescent cells and improved functional outcomes after IR in the brain. ABT263, a senolytic drug, is a novel therapeutic candidate for cerebral ischemia with IR injury.
Conclusion
Like all studies, this study has several limitations that should be noted when interpreting its results. Only astrocytes were used in the in vitro experiments, but many other cell types in the brain have been shown both to become senescent and to play a role in IR injury.
The authors also only used SA-ß-gal staining in vitro and only p16 in vivo to identify senescent cells. While both are very commonly employed, the senescent cell phenotype is complex and requires more than a single measurement to distinguish senescence from other cell fates. It is difficult to say for certain that these cells were senescent in these experiments.
This study also falls short in another common issue in aging research: their animals weren’t old. The rats were only 8-9 weeks old when they were treated. An aged rat (just like an aged human) might respond very differently both to IR injury and to the senolytic treatment.
Although many questions remain unanswered, this study is the first to demonstrate the potential role of senescent cells and of senolytic therapy in cerebral IR injury. The decreased infarction volume is particularly promising for the prospects of future research.
Literature
[1] Gorelick, P.B. The global burden of stroke: Persistent and disabling. Lancet Neurol. (2019). https://doi.org/10.1016/S1474-4422(19)30030-4
[2] Nour, M., Scalzo, F., & Liebeskind, D.S. Ischemia-reperfusion injury in stroke. Interv. Neurol. (2012). https://doi.org/10.1159/000353125
[3] Eltzschig, H.K. & Eckle, T. Ischemia and reperfusion—from mechanism to translation. Nat. Med. (2011). https://doi.org/10.1038/nm.2507
[4] Lim, S. et al. Senolytic therapy for cerebral ischemia-reperfusion injury. A meta-analysis of genome-wide association studies identifies multiple longevity genes. Int. J. Mol. Sci. (2021) https://doi.org/10.3390/ijms222111967