In a new paper, Ryan K. Masters, professor at CU Boulder, suggests that when adjusted for body shape and lifelong shifts, the relationship between BMI and mortality is more linear and robust than previously thought, with normal BMI being the healthiest [1].
BMI’s many problems
Most existing research shows a U-shaped relationship between body-mass index (BMI) and mortality, with slightly overweight people appearing to be the healthiest [2]. However, BMI is a flawed metric. In this new study, Ryan K. Masters from the University of Colorado Boulder attempted to account for those flaws and create a more precise model of association between BMI and mortality.
Among BMI’s many disadvantages is the fact that it does not account for body composition. As a result, muscular people can exhibit a higher-than normal BMI despite having low fat mass, while sarcopenic people with high fat mass can have normal BMI. We also know that not all fat is equally harmful, with visceral fat appearing to be the worst.
Another problem is that in populational research, BMI is rarely measured longitudinally. One measurement cannot tell the history of body weight fluctuations, which are highly relevant to future health. This creates two potential biases. First is the positive survival bias in high-BMI samples due to recent weight gain. This means that people who just recently became overweight or obese remain healthy for longer (“carrying over” their good health from when they had normal BMI to their new BMI category), thus lowering overall mortality for the high-BMI category.
The other side of the coin is the negative survival bias in low-BMI samples, which is caused by people who had lost weight due to illness (“reverse causation”). Their movement into the low-BMI category worsens outcomes there. Intentional weight loss contributes to the same effect: people who had been overweight for a long time and then lost weight tend to have the same health problems that they acquired during their period of obesity, even though they now reside in the low-BMI category. Simply put, it matters how much time a person spends with low or high BMI. This has also been shown by previous research [3].
Adjusting for BMI history and body composition
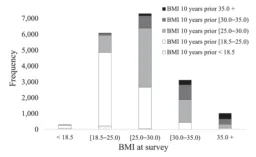
In his analysis, Masters used one of the best longitudinal health databases available, the American NHANES study, because it at least partially accounts for those factors. Many NHANES participants reported their previous body weight (10 years prior to the survey), and some body composition measurements were taken.
Using this previous reporting, Masters shows the amount of traffic between BMI categories. Unfortunately, if unsurprisingly, people more often acquire weight than lose it, with the overweight and obese categories heavily populated by people who previously had lower BMI:
Masters shows that the biases are real. The health of those who had moved to the normal BMI category from higher BMIs was much poorer than of those who had normal BMI both at the time of the survey and 10 years prior. Conversely, the health of those who had moved from normal BMI to being overweight or obese was generally better than of those who were stably in those two categories.
Lower-normal BMI wins
When Masters ran a model unadjusted for body composition and previous BMI, he saw the familiar U-shape, in which the lowest health risk was associated with being slightly overweight. However, when body composition and prior BMI were considered, the relationship became linear, with normal body weight being associated with least mortality. Both models were also adjusted for numerous potential confounding variables, such as socioeconomic status, smoking, and cardiovascular health. This is how it looks when normal body weight is chosen as the reference:
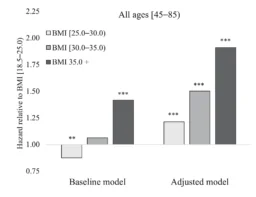
Masters then recalibrated his model for 9 different levels of BMI, with largely the same results. Here, what is generally considered normal BMI (18.5-25) was divided into three subcategories. People in the lowest subcategory (18.5-20) became the “golden standard” of health, with all other categories associated with higher mortality risk.
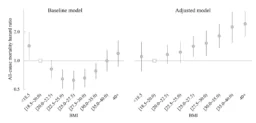
Notably, not only did the adjusted model show an almost linear relationship, but the effect sizes increased considerably, with people in the obese category being about twice as vulnerable as people with normal BMIs.
Conclusion
This study constitutes a commendable attempt to draw a more precise picture of the relationship between BMI and mortality by accounting for body composition and for lifelong shifts in BMI. Like every populational study, this one cannot establish causality. However, if taken at face value, it challenges the assumption that a bit of extra weight is good for your health. As more longitudinal health data continues to flow in, future studies should be able to further elucidate this important question.
Literature
[1] Masters, R. K. (2023). Sources and severity of bias in estimates of the BMI–mortality association. Population Studies, 1-19.
[2] Flegal, K. M., Kit, B. K., Orpana, H., & Graubard, B. I. (2013). Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. Jama, 309(1), 71-82.
[3] Preston, S. H., Mehta, N. K., & Stokes, A. (2013). Modeling obesity histories in cohort analyses of health and mortality. Epidemiology, 158-166.




