BioAge Labs: First Person Dosed in Phase 1 BGE-102 Trial
BioAge Labs, Inc. (Nasdaq: BIOA) (“BioAge”, “the Company”), a clinical-stage biotechnology company developing therapeutic product candidates for metabolic diseases by targeting the biology of human aging, today announced that the first participant has been dosed in a Phase 1 clinical trial evaluating BGE-102, a structurally novel, orally available small molecule NLRP3 inhibitor with high potency and brain penetration being developed initially for the treatment of obesity.
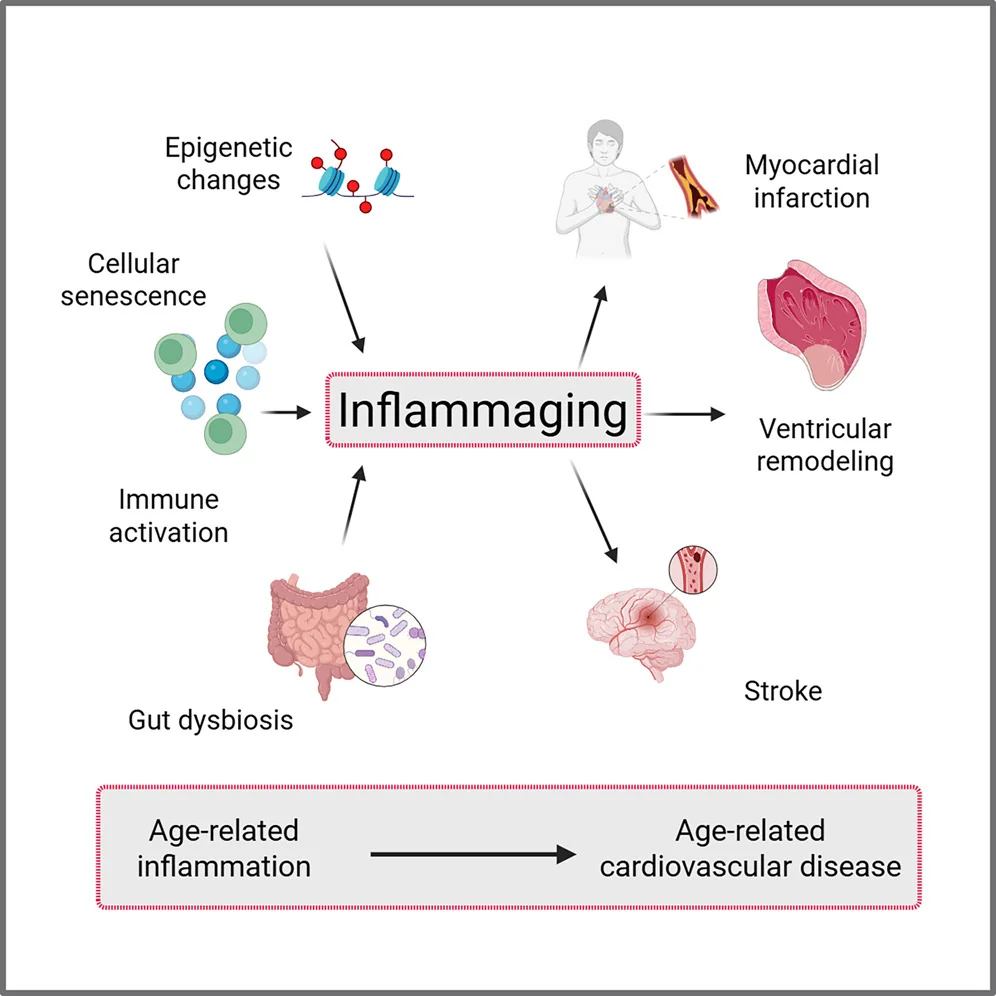
BGE-102 represents a structurally novel class of NLRP3 inhibitors developed by BioAge. NLRP3 is a key driver of age-related inflammation that has been implicated in a broad range of diseases, including neurodegenerative conditions and cardiovascular disease as well as metabolic disorders such as obesity. BioAge’s discovery platform identified NLRP3 as a therapeutic target based on analysis of human aging cohorts, which revealed that reduced NLRP3 activity is associated with greater longevity.
The Company’s research has shown that the new molecules inhibit the NLRP3 inflammasome through a unique binding site and mechanism distinct from other NLRP3 inhibitors in development [link, link]. The compound has demonstrated high potency consistent with once-daily oral human dosing along with high brain penetration, supporting its potential to address both neuroinflammation—which disrupts appetite regulation in the brain—and systemic inflammation associated with obesity and cardiovascular risk. BGE-102 has shown a strong safety profile in GLP toxicology studies that revealed no adverse findings [link].
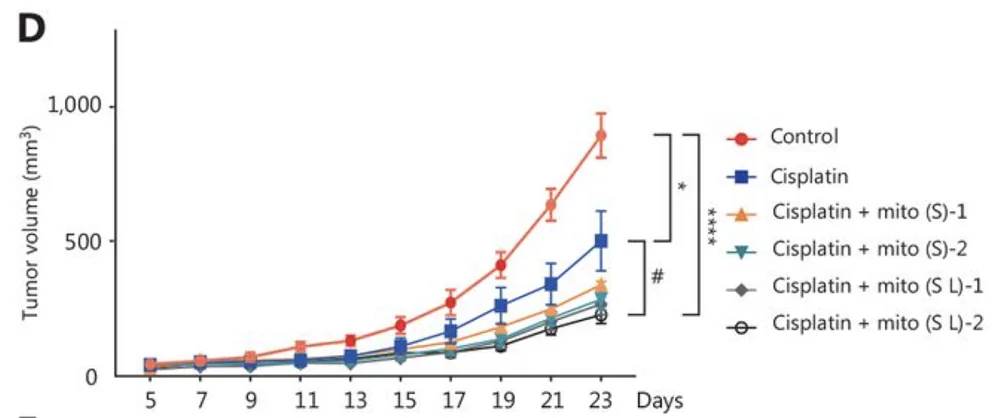
In preclinical obesity models, BGE-102 monotherapy achieved dose-dependent weight loss of up to 15%, comparable to semaglutide. When combined with semaglutide, BGE-102 produced additive effects, achieving approximately 25% weight reduction, supporting its potential application as part of an all-oral obesity regimen [link].
The Phase 1 study is a randomized, double-blind, placebo-controlled trial designed to evaluate the safety, tolerability, pharmacokinetics, and pharmacodynamics of BGE-102 in healthy participants. Part 1 will assess single ascending doses; Part 2 will evaluate multiple ascending doses administered once daily for 14 days. The study is designed to characterize BGE-102’s pharmacokinetic profile through blood sampling, assess CNS penetration through cerebrospinal fluid sampling, and evaluate pharmacodynamic effects using an ex vivo whole blood stimulation assay that measures BGE-102’s ability to inhibit the production of key inflammatory signals such as IL-1β.
“We’re excited to announce the dosing of our first participant in the Phase 1 trial for BGE-102 – a significant milestone in our mission to target the biology of aging and transform obesity treatment,” said Kristen Fortney, PhD, CEO and co-founder of BioAge. “This study was designed to deliver key data on safety, dosing, and activity. By inhibiting NLRP3-driven inflammation, a core driver of metabolic dysfunction, BGE-102 has the potential to complement existing therapies like GLP-1 agonists to enhance weight loss and curb excess inflammation. We believe that with convenient once-daily oral dosing and exceptional brain penetration, BGE-102 is positioned to tackle neuroinflammation in obesity and related conditions, offering versatility as a standalone or combination option.”
Following successful completion of the Phase 1 study, with initial SAD data expected by year-end 2025, BioAge plans to advance BGE-102 into a proof-of-concept study in obesity in 2026, with top-line data anticipated by end of year.
About BioAge Labs, Inc.
BioAge is a clinical-stage biopharmaceutical company developing therapeutic product candidates for metabolic diseases by targeting the biology of human aging. The Company’s lead product candidate, BGE-102, is a potent, orally available, brain-penetrant small-molecule NLRP3 inhibitor being developed for obesity. BGE-102 has demonstrated significant weight loss in preclinical models both as monotherapy and in combination with GLP-1 receptor agonists. A Phase 1 SAD/MAD trial of BGE-102 is underway, with initial SAD data anticipated by end of year. The Company is also developing long-acting injectable and oral small molecule APJ agonists for obesity. BioAge’s additional preclinical programs, which leverage insights from the Company’s proprietary discovery platform built on human longevity data, address key pathways involved in metabolic aging.
Forward-looking statements
This press release contains “forward-looking statements” within the meaning of, and made pursuant to the safe harbor provisions of, the Private Securities Litigation Reform Act of 1995. All statements contained in this press release that do not relate to matters of historical fact should be considered forward-looking statements, including, but not limited to, statements regarding our plans to develop and commercialize our product candidates, including BGE-102 and our APJ program, the potential for BGE-102 as a treatment for obesity and the expected timeline for data readout from our ongoing Phase 1 clinical trial, the timing and results of our clinical activities, risks associated with clinical trials, including our ability to adequately manage clinical activities, the timing of our IND filing for our APJ program, our ability to obtain and maintain regulatory approvals, the clinical utility of our product candidates or their ultimate ability to treat human disease, the expected timeline for completing proteomic analysis, anticipated analytical results and the potential for identifying novel therapeutic targets, and general economic, industry and market conditions. These forward-looking statements may be accompanied by such words as “aim,” “anticipate,” “believe,” “could,” “estimate,” “expect,” “forecast,” “goal,” “intend,” “may,” “might,” “plan,” “potential,” “possible,” “will,” “would,” and other words and terms of similar meaning. These statements involve risks and uncertainties that could cause actual results to differ materially from those reflected in such statements, including: our ability to develop, obtain regulatory approval for and commercialize our product candidates; the timing and results of preclinical studies and clinical trials; the risk that positive results in a preclinical study or clinical trial may not be replicated in subsequent trials or success in early stage clinical trials may not be predictive of results in later stage clinical trials; risks associated with clinical trials, including our ability to adequately manage clinical activities, unexpected concerns that may arise from additional data or analysis obtained during clinical trials, regulatory authorities may require additional information or further studies, or may fail to approve or may delay approval of our drug candidates; the occurrence of adverse safety events; failure to protect and enforce our intellectual property, and other proprietary rights; failure to successfully execute or realize the anticipated benefits of our strategic and growth initiatives; risks relating to technology failures or breaches; our dependence on collaborators and other third parties for the development of product candidates and other aspects of our business, which are outside of our full control; risks associated with current and potential delays, work stoppages, or supply chain disruptions, including due to the imposition of tariffs and other trade barriers; risks associated with current and potential future healthcare reforms; risks relating to attracting and retaining key personnel; changes in or failure to comply with legal and regulatory requirements, including shifting priorities within the U.S. Food and Drug Administration; risks relating to access to capital and credit markets; and the other risks and uncertainties that are detailed under the heading “Risk Factors” included in BioAge’s Quarterly Report on Form 10-Q filed with the U.S. Securities and Exchange Commission (SEC) on August 6, 2025, and BioAge’s other filings with the SEC filed from time to time. BioAge undertakes no obligation to publicly update any forward-looking statement, whether written or oral, that may be made from time to time, whether as a result of new information, future developments or otherwise.
Contacts
PR: Chris Patil, media@bioagelabs.com
IR: Dov Goldstein, ir@bioagelabs.com
Partnering: partnering@bioagelabs.com