Dr. Marco Quarta runs one of the most interesting start-ups in the longevity field: Rubedo, which focuses on utilizing the senolytic approach to cellular senescence. This company has developed ingenious ways to cope with the notorious heterogeneity of senescent cells and is one of the first to bring its senolytic drug candidate into clinical trials. Marco also co-founded Turn Biotechnologies, a company with a different vision based on partial cellular reprogramming, as he sees the future of anti-aging interventions as combinations of various drugs and therapies that tackle different aspects of aging.
Let’s start with how you got to where you are today.
My passion for the longevity field began when I was around five years old: I had this sudden inspiration that I wanted to become a scientist. With scientists and physicians in my family, it was natural inspiration, but what drove me was wanting to understand why different organisms live in different ways.
I had this realization that since we’re all made of the same matter, we should be able to change how long we live. It was naive, but that really inspired me. I never stopped; by age six, I had set up my first lab, playing with a chemistry kit and microscope with my family’s support.
I’m still exploring these questions today, perhaps less naively and more sophisticatedly. My studies and readings, not just in science but in philosophy, mythology, and history, were all about trying to understand this quest that humanity has pursued for millennia: how to live longer, healthier lives. The alchemist’s quest exists across all cultures and populations.
I think the difference now is that we now have real science. We’ve hit a tipping point where we have enough understanding, though there’s still much to learn, to move to Medicine 3.0 and develop longevity medicine.
As a quick side note, I actually wanted to ask you why your company Rubedo and its drug discovery platform ALEMBIC are named after alchemy terms.
I’ve long been interested in alchemy as a broader view of science and nature, a source of inspiration, essentially. Major scientists like Isaac Newton, the father of modern physics, and Robert Boyle, the father of modern chemistry, spent most of their careers as alchemists, trying to understand the language of nature and how it manifests in both animate and inanimate worlds.
There’s almost a spiritual dimension to science that has become disconnected from modern scientific practice, but philosophy and science have always been intertwined. Reading Persian, Arabic, Egyptian, Greek, Medieval, and Renaissance works, you find observational insights that remain inspiring for modern scientific approaches.
The names indeed come from alchemy. Rubedo is the final phase in creating the universal medicine, the elixir of long life meant to cure all diseases and extend longevity. Alembic was the apparatus alchemists used to distill and prepare this medicine, but ALEMBIC is also an acronym describing what our platform actually does: Algorithms for Life-Extending Medicine with Biology, Informatics, and Chemistry.
Okay, let’s go back to your story.
When choosing my university studies, I took this direction: aging biology. I did my undergraduate work in a lab under the patronage of the Nobel Laureate Rita Levi-Montalcini, who discovered nerve growth factor. I studied brain aging and regeneration, along with acute neuropathic pain. Then, I continued with a PhD in neuroscience, studying aging, physiology, and bioengineering. I wanted to understand aging from all angles, spending time on bioengineering, regenerative medicine, and stem cell biology.
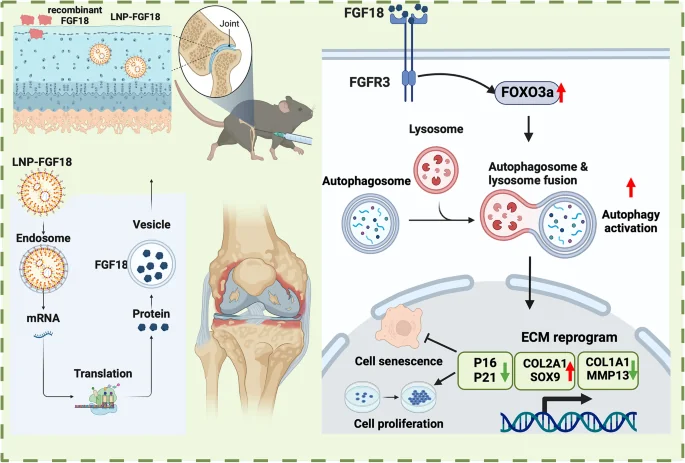
I came to Stanford to work with Thomas Rando, a pioneer in the field. It was a great environment to develop as a scientist. I went on to direct the research center for Tissue Regeneration, Restoration and Repair at Veteran Medical Center of Palo Alto and Stanford Medicine, leading a team working on regenerative medicine, bioengineering, stem cells, aging, and rejuvenation in different areas. Our work on epigenetic reprogramming along with the lab of Vittorio Sebastiano, also at Stanford, became the foundation of Turn Bio.
Yes, it is interesting that you’re also a co-founder in a cellular reprogramming company
Aging is complex, but what we could do immediately is remove pathologic cells, like we have been doing for cancer for the past 50-60 years. You can’t live with them. Now we know there are other pathologic cells, more age-related, such as senescent cells, but, like cancer cells, they are highly heterogeneous. Also, they’re not all bad, but rather pleiotropic, they have different states.
The field is exciting because it reminds me of oncology in the 60s-70s. Back then, people naively wanted to develop chemotherapies to kill all cancer cells. After 50 years, we have cures for some cancers, we’re still working on others, and we understand how complex it is – we need multiple therapies and modalities.
A lot of it is the same for cellular senescence, which is why I started Rubedo: we needed to build tools first to understand the differences in cells. The idea is to remove the pathologic cells that emerge with aging biology. The other approach, with Turn Bio, is to preserve or restore useful biology in aging cells that are becoming dysfunctional – turning back the clock using cellular reprogramming.
I see strong synergy between these two strategies and platforms. My hope is that in the future, these therapies can work together for a truly comprehensive longevity approach, rather than just treating diseases of aging as we’re doing now. The field is changing and advancing quickly.
I founded the Phaedon Institute a couple of years ago with several key opinion leaders from academia and industry. We have members from leaders in academics, industry. The goal is to raise awareness, improve scientific rigor, help the field advance, create winners. I see the field made of collaborators, not competitors. If someone succeeds, everybody will benefit. So, it’s important that we create this ecosystem. It’s a complex mission but advancing very quickly.
Since you mentioned the Phaedon Institute, tell me more about it. I think it’s an interesting organization that’s been largely flying under the radar.
We’ve been working more behind the scenes. This year, we’re organizing the new Senotherapeutic Summit. The last one was in 2023 – we hold it every two years, as we believe annual meetings don’t allow enough progress. This year, it will be combined with the International Cellular Senescence Society for a longer meeting combining academic work, industry, and clinical perspectives. It will be held in Rome in September.
We’ve been creating a framework to help advance the field and coordinate different aspects from education to research to investments. Our goal is to have focused activities rather than constant PR. We’re planning another event focused on epigenetic reprogramming and other aspects of aging. I’m not a fan of the “hallmarks of aging” framework, but we want to understand different areas separately rather than mixing them all together, having different communities work on different aspects.
Let’s move on to Rubedo. The year 2024 was really busy for you, right? You closed funding series for 40 million dollars, you signed a lucrative partnership, you’re gearing up for your first human trial, and you also have a new CEO. Tell me all about it.
We actually ended up raising 46 million after the announcement as more investors wanted to join. Part of this came from CDP Ventures, a major Italian investment fund – essentially a government sovereign fund that drives innovation. This supported our expansion into Italy, where we opened an office in Milan. We chose Milan as our European headquarters not just for our upcoming clinical trial in the Netherlands, but with the goal to eventually expand our R&D operations across Europe. We announced the target of the first program going to the clinic now.
And you chose skin indications – atopic dermatitis, psoriasis – correct?
Yes, among other chronic inflammatory skin diseases and skin aging, we chose the skin as the tip of the spear, an entry point. While we’ve been investigating many therapeutic areas – muscle, brain, liver, lung – we found skin to be the most accessible starting point. It allows us to move quickly in multiple directions.
This trial gives us a unique opportunity to study aging in a clinical setting through a basket trial approach, starting immediately with patients in a Phase 1. Skin is ideal because you can directly observe and assess it. We received approval for a Phase 1 trial primarily testing safety, but we’ll be treating multiple patients with chronic inflammatory skin conditions that we’ve carefully profiled in parallel with skin aging. We’ve analyzed clinical samples using our ALEMBIC platform, incorporating single-cell RNA sequencing, multi-omics, spatial transcriptomics, and AI integration to identify senescent cell types and potential targets.
These are great market opportunities – some are still unmet medical needs predicted to become blockbuster markets. Guggenheim’s end-of-year forecast surprisingly placed dermatology at the top of therapeutic areas, which aligns with our pipeline indications. Strategy& flagged an analysis that forecast senotherapeutics to be at $127B market by 2030.
We’ll be studying target engagement, biomarkers, and various changes. Beyond examining biopsies of diseased tissue, we’ll also analyze normal aged skin to look not just at disease biomarkers but at changes in skin aging biology – including epigenetic clock measurements and specific aging markers. This makes it a true dual-purpose trial examining both therapeutic effect and aging processes.
As you said, we also closed a major deal with Beiersdorf, one of the largest cosmetics companies globally, known for brands like Nivea, Coppertone, and Eucerin. We’re collaboratively developing anti-aging skincare that actually rejuvenates the skin – not just marketing, but creating genuinely healthier, younger skin.
As we move into the clinical stage, I wanted to focus more on innovation and R&D for our new programs, so I looked for someone to complement my work. We found Frederick Beddingfield, who was an ideal fit. He’s a dermatologist with a PhD who became an executive, serving as CMO at Allergan where he launched several drugs including Botox for medical aesthetics and therapeutics. He’s had successful CEO roles in several companies, including one he sold back to Allergan for 2.2 billion, and has led multiple IPOs.
The last two years, Beddingfield worked as a venture capitalist at Apollo Health Ventures, focusing on longevity therapeutics. When he saw our work, his words were, “I can’t say no here.” He brings the experience to build our clinical strategy with the understanding that we’re not just a dermatology company – we’re a longevity company, and skin is just our starting point.
Tell me more about your target.
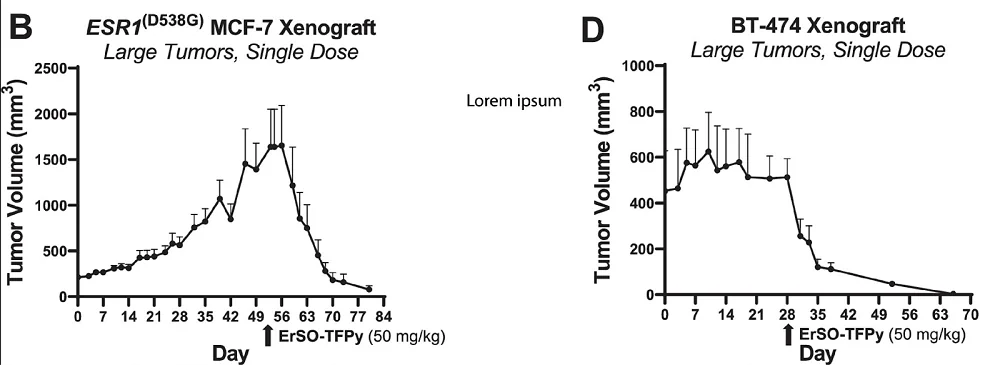
We just announced our target during the JP Morgan conference: it’s GPX4. Our compound RLS1496 is a proprietary GPX4 modulator. We developed a molecule that can modulate GPX4 and target vulnerabilities in senescent cells while sparing healthy cells, and its effects extend beyond skin.
GPX4 is central to ferroptosis, a distinct form of cell death different from apoptosis or necroptosis. Though this pathway was only discovered about ten years ago, it’s generating a lot of interest. Major companies like Takeda, Bayer, and Calico (in collaboration with AbbVie) are working on it.
This target has been studied mostly in the context of oncology so far. Now, people are looking at cardiovascular conditions, inflammation, and fibrosis. Our own next step will be systemic applications targeting inflammation and metabolic disorders. We also have other programs with different targets – for instance, our lung interstitial disease program, supported by the California Institute for Regenerative Medicine (CIRM), targets lung stem cells that become senescent. These cells trigger a cascade leading to fibrosis as in IPF, and tissue degeneration leading to COPD or pulmonary hypertension. We’ll start with lung fibrosis before expanding to other indications.
In oncology, ferroptosis has been explored as a therapeutic opportunity studying aggressive cancer cells that resist traditional treatments. Researchers are trying to use synthetic lethality approaches to sensitize treatment-resistant cancer cells to ferroptosis, with GPX4 as a target. This presents challenges because cancer cells proliferate rapidly, develop resistance, and require carefully engineered synthetic lethality.
What we discovered is that certain senescent cells are naturally vulnerable to ferroptosis. But senescent cells have an advantage over cancer cells – they don’t divide or grow. This means we can use more flexible dosing schedules and don’t need to eliminate every single cell immediately. We can gradually reduce their population over time.
In the case of ferroptosis, researchers found they could make cancer cells more sensitive to this type of cell death by inhibiting CDK4/6 with drugs like palbociclib. What makes senescent cells particularly interesting is that they have a natural predisposition to this sensitivity. When cells become senescent, they can elevate levels of p16 and/or p21, which are natural inhibitors of CDK4/6, creating an almost built-in synthetic lethality mechanism.
We’ve found that by modulating GPX4 in specific ways, we can trigger ferroptosis in senescent cells while sparing healthy cells, giving us a therapeutic window. Our compound, RLS1496, is a potent GPX4 modulator that can achieve this effect at single-digit nanomolar concentrations.
Studies have shown that reducing GPX4 levels throughout life in mice (not completely removing it, which is lethal at birth) increases lifespan by 7-10%, and these mice develop fewer tumors and are generally healthier. While this suggests a broader role in longevity, we’re currently focusing on targeting specific pathological senescent cell populations.
This brings up an interesting question about the notorious heterogeneity of senescent cells. Are you targeting specific subsets of senescent cells, and is your ALEMBIC platform designed to address this heterogeneity problem?
Yes, exactly. Senescent cells come in different types and flavors, but unlike cancer cells that keep dividing and developing resistance, senescent cells maintain relatively stable states once established. The type of senescence depends on the initial trigger: different stressors lead to different senescent states. Cell types also acquire different senescent states depending on their tissue of origin and the disease context. Once you identify these distinct populations, you can target them specifically, and you don’t need to eliminate them all at once.
The challenge was how to identify and characterize these different populations. When we started Rubedo, the tools to address this complexity didn’t exist. That’s why we developed ALEMBIC, which is built on single-cell multi-omics technology. This is a relatively new frontier – even ten years ago these technologies didn’t exist, but now they’re becoming mainstream.
We began with single-cell RNA sequencing and have since incorporated ATAC sequencing, genomics, and spatial multi-omics, continuously adding layers of data. We source our samples directly from patients – such as skin biopsies, lung tissue from IPF patients at Cedars Sinai Medical Center in LA, and samples from COVID patients with interstitial lung diseases.
These patient samples are our starting point for data generation. To make sense of this complex data, we use deep neural networks and machine learning algorithms that we’ve developed in-house. Just as we create our own molecules rather than repurposing existing drugs, we build our own computational tools.
The discovery component of ALEMBIC uses algorithms trained on our large in-house datasets. These can analyze samples and triangulate across different cell types to identify senescent states, their various subtypes, and potential biomarkers or signatures. We’re now developing different modalities that take advantage of vulnerabilities identified with ALEMBIC. An example of such targeted modalities are prodrugs based on this understanding – creating inactive senolytics with specific modifications that are only activated by enzymes present in senescent cells. This improves our safety profile.
Through ALEMBIC, we’re discovering novel enzymes, mechanisms, and pathways specific to certain senescent cell populations. This requires understanding cellular states at single-cell resolution across healthy and diseased tissue, different ages, and how various cell types interact. This forms the foundation of ALEMBIC. We then leverage a chemistry platform that translates these insights into molecules, using both in silico simulation and generative chemistry approaches specifically designed for targeting senescent cells or pathologically aging cells. Using these approaches to support our medicinal chemistry to optimize lead molecules, we accelerate and inform our drug discovery and development, derisking the process.
We’ve seen a couple of early failures in senolytic clinical trials. Does this concern you? Everyone was excited about senolytics as a low-hanging fruit, but it’s proved more complex than anticipated.
I always look back to the early days of oncology and how many therapies failed before we started seeing success. Now, we have cures for certain cancers. Clinical trials are experiments in humans – as a scientist, I know you design them as carefully as possible but like in any experiment, failure is part of learning how to redesign and recalibrate.
The field of senolytics started with great excitement but perhaps moved too quickly. You’re probably talking about UNITY’s first trial, followed by another in 2023. I believe they chose an interesting target but in a challenging indication as their starting point. Their trial design was also complicated – a single intra-joint dose followed by a 12-week wait to assess pain scores, which are inherently noisy measurements. Additionally, the trial coincided with COVID’s onset, leading to significant patient dropout and loss of statistical power.
The results were ultimately inconclusive. One limitation was their choice of a BCL-2/XL inhibitor, which comes with toxicity issues from its oncology origins. This first-generation senolytic has systemic limitations like thrombocytopenia that need addressing for systemic use. They’ve since shifted to localized delivery, first in joints for arthritis and now in the eye.
Their recent trials in diabetic macular edema are actually quite exciting. A single intraocular injection showed functional improvements in visual acuity over twelve months. Compare this to standard VEGF inhibitors that require injection every three to four months – I’ve seen how difficult this is, as my father had this condition. Their results show that removing senescent endothelial cells from the eye with a single treatment could provide superior and potentially long-lasting results to current standard of care.
On the other side, we’re seeing promising results from academic trials, like those at Mayo Clinic. While they’re using less selective senolytics like dasatinib plus quercetin – essentially repurposed chemotherapy – they’re showing effects. Their studies in IPF patients, kidney diseases, preeclampsia, diabetes, and cancer are demonstrating reduced senescence, decreased inflammation, and functional improvements. Ongoing trials are assessing senolytic interventions for frailty, Alzheimer’s, chronic kidney diseases, and other neurodegenerative conditions, to name a few.
The Mayo Clinic’s IPF open-label pilot trial is particularly noteworthy. Despite being a small trial with a challenging patient population, they showed improved function, quality of life, such as six-minute walk distance and four-minute gait speed. Current approved drugs for IPF – nintedanib and pirfenidone – slow down fibrosis and extend survival for some patients, but at the cost of quality of life. They’re so toxic that patients often choose to discontinue treatment despite having only 2-3 years life expectancy at diagnosis. Even the relatively crude combination of dasatinib plus quercetin improved quality of life in these patients. This suggests we’re on the right track: we just need to learn from the biology and refine our therapeutic approaches.
You’ve said that senescent cells are key drivers of chronic diseases, from cancer to cardiovascular disease, dementia, and diabetes. How fundamental is cellular senescence as a cause of aging?
Aging is a complex systems problem – that’s why I don’t like the “hallmarks of aging” framework. All components are interconnected; when one thing changes, everything responds. But senescence is a particularly interesting integration point for cellular dysfunction. It can arise from DNA damage, mitochondrial dysfunction, telomere attrition, epigenetic changes, and other causes. It’s fundamentally a defensive response – when something’s wrong, cells stop dividing and start secreting signaling factors (SASP).
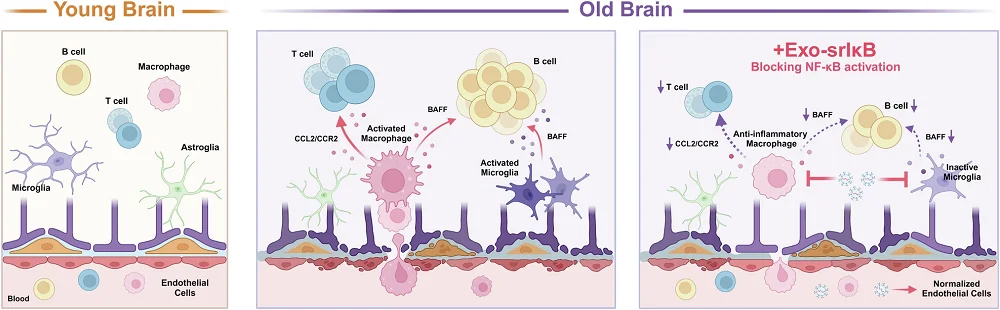
This process is actually beneficial in certain contexts: during development, embryogenesis, and wound healing. These factors help recruit immune cells and modulate tissue responses, supporting regeneration when working properly. It’s a pleiotropic biology with two faces. Problems arise when these cells escape immune surveillance and accumulate, sending aberrant signals to immune cells and stem cells. They create a maladaptive response where inflammation becomes chronic and self-perpetuating.
So, senescence is a response to damage and stress. It’s part of aging, because over decades we accumulate damage and lose our capacity to buffer these responses, but this isn’t just about chronological aging. Consider children with leukemia undergoing chemotherapy – they show very high levels of inflammation and senescence markers. Cancer survivors, including pediatric patients, often develop age-related diseases decades earlier than average. It’s an acceleration of the normal aging process.
COVID-19 provided another example: SARS-CoV-2 causes senescence in epithelial cells. At Cedars, we’re seeing people in their 40s in need of lung transplants, with lung tissue aging phenotypes equivalent to typical 70-year-old IPF patients. Senescent cells both accelerate aging and are produced by aging, creating an amplifying cycle.
Removing senescent cells breaks this cycle and clears tissues of factors that drive chronic inflammation. They’re not the only source, but they’re a persistent one. Consider current treatments for severe dermatological conditions like psoriasis or atopic dermatitis – these biologics target single factors like TNF-alpha, IL-17, IL-23, or IL-6, which are all SASP components. Instead of targeting individual factors, we can remove their source upstream and let immune cells and stem cells to restore normal function.
This process happens in disease but also in healthy aging, with gradual degeneration and loss of tissue function. Removing senescent cells isn’t the only solution, but it’s an important part of the longevity medicine toolkit. After removing these cells, you can apply other interventions: epigenetic reprogramming, improving mitochondrial function, remodeling the extracellular matrix. These therapies could eventually be personalized and combined.
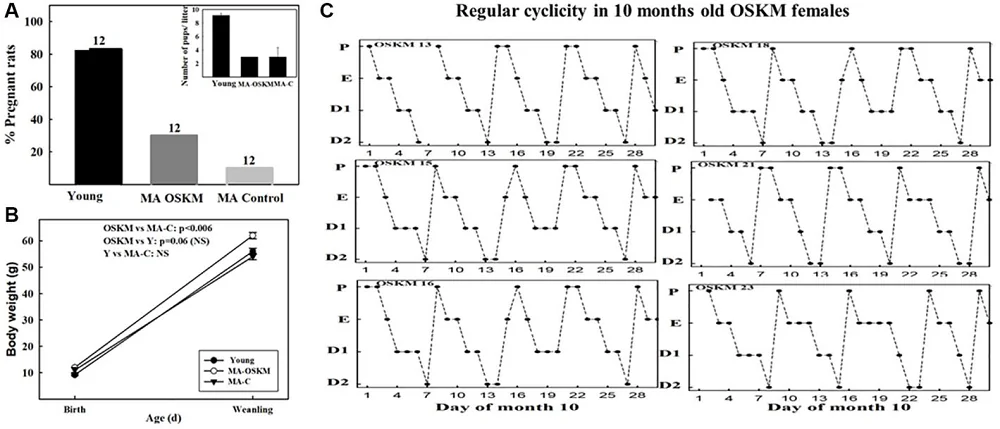
The importance of senescent cells in driving premature aging has been demonstrated experimentally – we’ve shown this too. Transplanting senescent cells, whether from humans into mice or between mice, causes premature aging. Even a small number of these cells can drive frailty and age-related symptoms. Moreover, Campisi and Conboy’s lab’s elegant work showed that exposing young mice to even a single exchange of blood from aged mice accelerates aging and induces cellular senescence prematurely. Conversely, this induction of cellular senescence is abrogated if the old mice are pre-treated with senolytic drugs, suggesting that cellular senescence is neither a simple stress and damage response nor a chronological cell-intrinsic phenomenon.
This transition to human applications is just beginning. In conditions like IPF, the role of senescence is becoming clear. Evidence from 15 years ago showed that the primary problem isn’t fibroblasts causing fibrosis – it’s upstream, where epithelial progenitors and stem cells lose their healing capacity, especially in patients with genetic predispositions like telomere mutations.
When you add environmental stress – smoking, pollution, COVID – this triggers a strong and persistent cellular senescent response. You lose functional progenitors and stem cells, which are replaced by senescent cells that perpetuate the cycle and activate aberrant immune responses. The resulting pro-inflammatory, pro-fibrotic environment activates fibroblasts to become myofibroblasts, leading to collagen deposition and scarring. Breaking this cycle by removing senescent cells could lead to disease-modifying treatments.
We’re about to publish work in an important peer-reviewed scientific journal with Stanford collaborators showing how cellular senescence influences chronic pain development: neurons become senescent after injury, spread senescence to surrounding neurons, and drive the transition from acute to chronic pain. Removing senescent cells can reverse this process.
So, you believe that senolytic therapies should be customized to specific disease conditions, perhaps even individual patients, and that longevity medicine will eventually involve multiple simultaneous approaches. Can you elaborate on this vision?
The future of longevity medicine doesn’t necessarily require customization to individual patients for senolytics. Rather, we need to understand how single therapies can be applied across multiple diseases and patient groups. We also need to identify the best responders and how to stratify patients effectively. That’s for treating existing diseases.
The next frontier is prevention: understanding how to remove specific senescent cell populations before disease develops. This isn’t possible yet because we need validated biomarkers, which we’re working to develop in our trials.
I envision a future where you visit your doctor for routine tests, and just as they now tell you when your glucose or HbA1c levels indicate pre-diabetes, they’ll check a panel of senescence markers. They might tell you that you have concerning senescence levels in your liver and recommend specific interventions to prevent conditions like NASH from developing 10-20 years later.
As we learn more, we’ll understand which treatments work best for particular marker patterns, whether used alone or in combination. But first, we need to validate these therapies and understand how they work. Look at GLP-1 drugs: there’s tremendous excitement, but we’re still learning about different patient responses and side effects. That’s just how medicine and drug discovery work.
We can accelerate this process with modern tools like AI, de-risk development, and speed up pipelines, but we still need to follow the scientific journey. Unfortunately, the current drug development process isn’t well-suited to preventive medicine. Drug development faces multiple challenges – market penetration, payer acceptance, physician and patient adoption. The marketing aspect isn’t just about sales but creating awareness and changing habits.
We often see improved medicines fail simply because patients stick with familiar treatments, missing potentially life-changing opportunities. These become sleeping assets in pharmaceutical companies, perhaps to be rediscovered later for different purposes.
That’s why advocacy is crucial, creating awareness about longevity medicine, educating physicians and policymakers, and preparing society for this medical paradigm shift. As we develop new therapies, we need a society ready to understand and implement them.
We would like to ask you a small favor. We are a non-profit foundation, and unlike some other organizations, we have no shareholders and no products to sell you. All our news and educational content is free for everyone to read, but it does mean that we rely on the help of people like you. Every contribution, no matter if it’s big or small, supports independent journalism and sustains our future.









 nst disease and the persistent ravages of aging?
nst disease and the persistent ravages of aging?