How Extracellular Vesicles From Stem Cells Fight Senescence
Researchers have discovered a cocktail of micro-RNA strands that make some extracellular vesicles (EVs) effective in reducing cellular senescence and published their findings in Aging Cell.
A new approach to senescence
Read More
The researchers began their paper discussing the well-trodden ground of senolytics, which kill senescent cells, and senomorphics, which alter them instead. They noted that cellular senescence is often targeted in aging because it is presumably easier to drug than other aspects are, and they listed various senolytics and senomorphics, such as fisetin and the well-known combination of dasatinib and quercetin. They even noted rapamycin’s senomorphic qualities [1].
However, they have chosen a different, and possibly more effective, approach. EVs are signaling molecules sent from one cell to another, and they contain various molecules that control how cells behave. We have reported on researchers finding EVs to be effective against a variety of conditions, such as enlarged hearts, and even extending lifespan in mice. With an eye towards how they affect senescent cells, these researchers took a look at EVs in depth, attempting to find which of their components, specifically micro-RNA strands (miRNAs), lead to such benefits.
A variety of EVs demonstrate benefits
This study began by driving fibroblasts senescent through etoposide for 48 hours, then removing it and waiting for six days. The researchers then confirmed that EVs derived from stem cells, including embryonic stem cell-derived vesicles (AC83) known to be effective in mice, reduce the senescence of these cells. EVs from endothelial stem cells, different embryonic progenitor stem cells, and human liver stem cells were all compared to AC83 and a control group.
All of these cells had some degree of statistically significant effect, although AC83 appeared to be slightly more effective than the other types in rapidly reducing the proportion of senescent cells, from 100% to approximately 70%, as measured by SA-β-gal. Other senescence biomarkers, including p16, p21, and the inflammatory interleukins IL-1β and IL-6, were also reduced, although AC83 was the only one to reduce p21 and the human liver stem cells were the least effective overall.
Critically, they were all found to be senomorphic rather than senolytic; the number of total cells did not significantly decrease due to EVs derived from any source.
Looking for the right combination
The next step was to take a look at the specific miRNAs involved. Using the miRNA Enrichment Analysis and Annotation Tool (miEAA) and an age-related genetic database called GenAge, the researchers sought to determine which of the miRNAs they extracted from their EVs might be having these beneficial effects, intentionally filtering out miRNAs that also appear in EVs derived from non-stem cell fibroblasts. They found eight different ones that scored highly based on this metric.
Interestingly, none of these miRNAs had complete benefits on their own. One compound decreased SA-β-gal but significantly increased inflammatory interleukins. Another compound did nothing to SA-β-gal but decreased these interleukins. One miRNA that decreased senescence also decreased p16 but provided no benefits elsewhere.
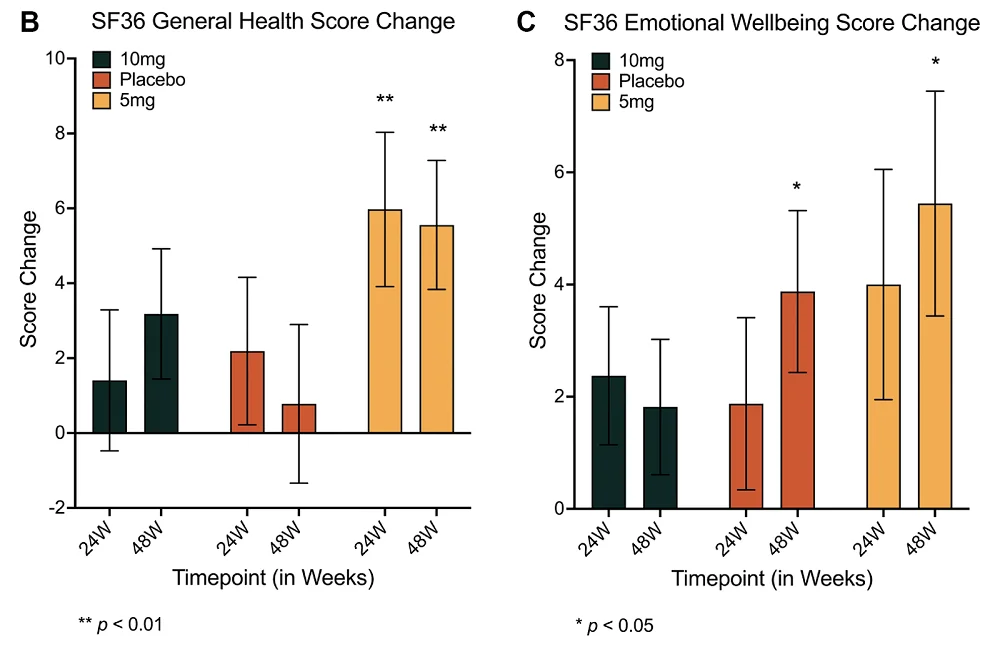
Intrigued by these results, the researchers began testing various combinations and screening them for effectiveness. After multiple attempts, they found that a combination of four of these miRNAs (E5) was sufficient to have broad, positive effects on senescent fibroblasts, reducing the senescent proportion even more than AC83 and having broad benefits against inflammation and other senescence markers.
A genetic investigation found a potential reason why this is the case. Specifically, the genes PCAF and HIPK2 work together to activate p21 in response to genetic damage, beginning a senescence response. These genes were downregulated by E5 at different times, apparently blocking this source of senescence. E5 was also found to affect multiple other pathways, including those related to inflammation, mTOR, and the cell cycle.
Effectiveness in mice
Unsuprisingly, the expression of all four of the E5 miRNAs was downregulated in old mice compared to young mice. To determine its possible therapeutic effectiveness, the researchers injected two-year-old mice with E5 three times over two weeks. They found that, in liver tissue, there was a reduction of both senescence and a DNA damage marker along with reductions in other senescence markers. Inflammation markers trended toward reduction, and the difference was barely outside of statistical significance.
There were several aspects of these miRNAs that went unexplored; for example, it is not known what precise effects they had on other types of cells, and this paper did not include a lifespan study. It may be that miRNA cocktails that specifically instruct cells not to become senescent, delivered through nanoparticles or genetated EVs, may be more potent than senolytic or senomorphic small molecules. Significant work needs to be done to determine the extent of miRNAs’ potential effectiveness.
Literature
[1] Selvarani, R., Mohammed, S., & Richardson, A. (2021). Effect of rapamycin on aging and age-related diseases—past and future. Geroscience, 43, 1135-1158.