Researchers have recently published a review on how cannabis use among older adults impacts age-related conditions and longevity [1].
Cannabinoids and longevity
In recent years, researchers have observed an increase in cannabis use among older adults, mostly for chronic conditions, such as arthritis, pain, sleep improvement, anxiety, and depressive symptoms.
However, there is also a recent interest in using cannabis-derived cannabinoids, especially cannabidiol (CBD) and Δ9-tetrahydrocannabinol (THC), as potential anti-aging and longevity-promoting treatments.
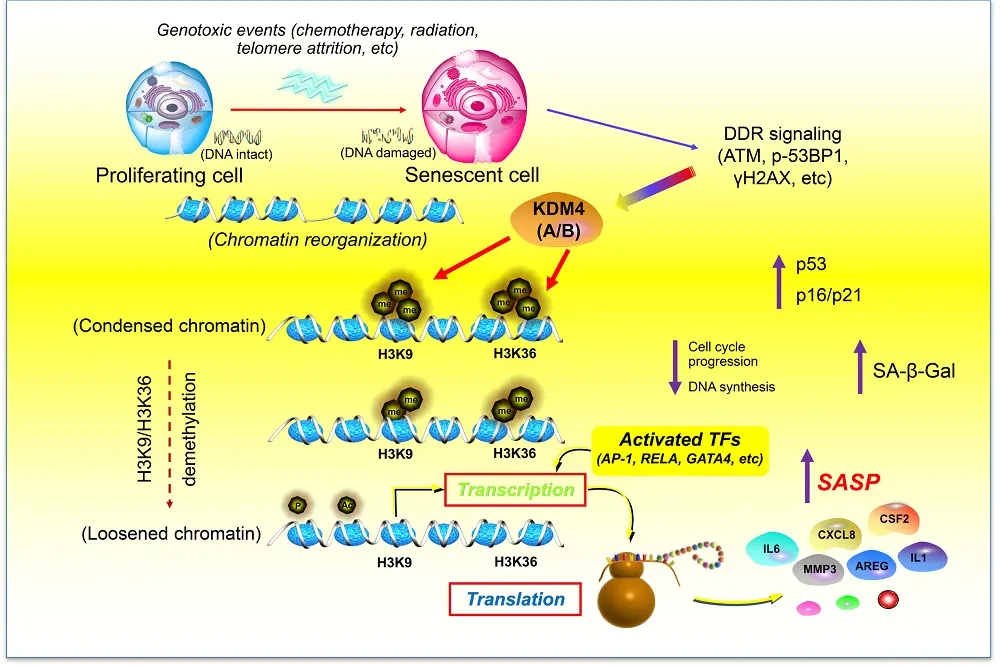
CBD and THC interact with the endocannabinoid system (ECS), which has been linked to impacting aging and longevity [2]. While the researchers do not have a detailed understanding of how the endocannabinoid system interacts with cannabinoids to promote health and longevity, the reviewed studies suggest that cannabinoids might promote cellular homeostasis.
This review encompassed what is currently known about the cannabinoids’ anti-aging properties, as well as their limitations, drawbacks, and side effects. The reviewers excluded studies whose focus was on the acute effects of cannabis or its action in different medical conditions. They found 11 preclinical and 7 human studies that met their search criteria.
Promising animal data
Most of the early studies regarding biological questions are done in model organisms. This is also the case for cannabis, as the researchers utilized worms, fruit flies, zebrafish, and mice to analyze its connection to health and lifespan outcomes.
Worm and fruit fly studies show that CBD and THC exposure can lead to lifespan extension, improved neuronal health, delayed age-related neurodegeneration, and increased autophagy. However, the beneficial effects often depend on using a specific dose of cannabis [3-6].
Another model organism that was used for cannabis research is the zebrafish, as its endocannabinoid system is well conserved, meaning it shows high similarity to humans. A study that analyzed the impact of THC exposure during development pointed to the dose-dependent differences, with lower doses leading to increased male survival and egg production, and reduced markers of aging and inflammation in the liver. Higher doses had negative consequences for offspring, survival, and reproduction [7].
Mice’s endocannabinoid systems are also similar to those of humans. In older mice, lower doses of THC led to improvements in memory and reversal of cognitive decline; however, this was not the case for THC-treated younger animals, which showed a decline in cognitive performance [8].
Cognitive performance improvements were also seen in two different studies where older mice were either chronically (for 28 days) exposed to a low dose of THC [9] or received a single injection of an extremely low THC dose [10]. Similarly, the memory and brain health of aged mouse models of Alzheimer’s disease benefited from intranasal low-dose THC treatment [11].
A mouse study also pointed to potential interactions between THC and CBD, as a low dose of THC was beneficial for spatial learning in aged mice, but when combined with CBD, the beneficial effect was not present [12]. This study points to the importance of further investigation into the combined effects of different cannabinoids.
The human data
While the evidence from model animals is promising, it needs to be confirmed in human studies, which are mostly lacking, and existing results are inconsistent. The human studies show a difference in outcomes regarding the age at which people started to use cannabis and how long they have been taking it. Several studies that examined people who used cannabis during adolescence and/or engaged in long-term use found that they had worse executive function, reduced grey matter, poorer verbal memory, accelerated biological aging, and worse health [13-16].
The effects are different when cannabis is taken by the elderly. For example, a study that included older adults, aged 60-88, who used cannabis weekly for at least the past year, showed increased connectivity in several brain regions, suggesting improved communication and information processing [17].
However, another study of people at least 60 years old showed lower executive functions in long-term cannabis users compared to non-users or short-term users. Short-term use didn’t seem to impact cognitive performance in this study [18].
Since there is a shortage of human studies on cannabis, the researcher also examined evidence regarding cannabis-based medicinal products (CBMPs) among older people. The data suggest CBMPs’ potential in treating aging-associated conditions, such as insomnia, depression, anxiety, and chronic pain. Cannabis use can also help reduce opioid dosage [19].
In total, the data from human studies and observations show age-dependent effects of cannabis. When cannabis use is initiated early in life, it leads to cognitive impairment later in life, but initiating cannabis use later in life shows more promising outcomes; however, there is still a need for more investigation in people.
The authors believe that some of the opposing age-dependent effects of cannabis might be caused by the changes that occur to the endocannabinoid system as it ages, such as changes in receptor binding and gene expression.
While analyzing different studies, the authors noticed methodological issues in human studies investigating cannabis use. First, the dose reporting is inconsistent and reports broad terms such as “heavy” or “recreational,” but no precise measurements are given. Second, there is a generalization of age categories, such as “older adults.” Both of those make interpreting the results and drawing strong conclusions harder. However, those researchers point out that they used those studies to gain an understanding of broader trends.
The authors also point out that there are differences in cannabis use patterns among the older population, with some people being new users (people who started after 60), while others are intermittent or consistent users. Those differences make cannabis research use more complex, as the effects of cannabis in each group might be different, and optimal therapeutic approaches might differ.
Cautious optimism
While most of the reviewed results seem to be optimistic, they should be interpreted with caution, as they are scarce and have many limitations. Additionally, most human studies are observational and cannot establish a causal link.
In the future, there is a need for well-designed human trials to understand the effect of cannabis on health and longevity, the consequences of the long-term effects of cannabis use among the elderly, and the effect of different dosing and routes of administration. There is also a need to investigate other cannabinoids beyond THC and CBD along with their interactions with each other and other medications and compounds.
We would like to ask you a small favor. We are a non-profit foundation, and unlike some other organizations, we have no shareholders and no products to sell you. All our news and educational content is free for everyone to read, but it does mean that we rely on the help of people like you. Every contribution, no matter if it’s big or small, supports independent journalism and sustains our future.
Literature
[1] Nain, S., Singh, N., Schlag, A. K., & Barnes, M. (2025). The impact of cannabis use on ageing and longevity: a systematic review of research insights. Journal of cannabis research, 7(1), 52.
[2] Paradisi, A., Oddi, S., & Maccarrone, M. (2006). The endocannabinoid system in ageing: a new target for drug development. Current drug targets, 7(11), 1539–1552.
[3] Land, M. H., Toth, M. L., MacNair, L., Vanapalli, S. A., Lefever, T. W., Peters, E. N., & Bonn-Miller, M. O. (2021). Effect of Cannabidiol on the Long-Term Toxicity and Lifespan in the Preclinical Model Caenorhabditis elegans. Cannabis and cannabinoid research, 6(6), 522–527.
[4] Wang, Z., Zheng, P., Chen, X., Xie, Y., Weston-Green, K., Solowij, N., Chew, Y. L., & Huang, X. F. (2022). Cannabidiol induces autophagy and improves neuronal health associated with SIRT1 mediated longevity. GeroScience, 44(3), 1505–1524.
[5] Wang, Z., Zheng, P., Xie, Y., Chen, X., Solowij, N., Green, K., Chew, Y. L., & Huang, X. F. (2021). Cannabidiol regulates CB1-pSTAT3 signaling for neurite outgrowth, prolongs lifespan, and improves health span in Caenorhabditis elegans of Aβ pathology models. FASEB journal : official publication of the Federation of American Societies for Experimental Biology, 35(5), e21537.
[6] Candib, A., Lee, N., Sam, N., Cho, E., Rojas, J., Hastings, R., DeAlva, K., Khon, D., Gonzalez, A., Molina, B., Torabzadeh, G., Vu, J., Hasenstab, K., Sant, K., Phillips, J. A., & Finley, K. (2024). The Influence of Cannabinoids on Drosophila Behaviors, Longevity, and Traumatic Injury Responses of the Adult Nervous System. Cannabis and cannabinoid research, 9(3), e886–e896.
[7] Pandelides, Z., Thornton, C., Lovitt, K. G., Faruque, A. S., Whitehead, A. P., Willett, K. L., & Ashpole, N. M. (2020). Developmental exposure to Δ9-tetrahydrocannabinol (THC) causes biphasic effects on longevity, inflammation, and reproduction in aged zebrafish (Danio rerio). GeroScience, 42(3), 923–936.
[8] Bilkei-Gorzo, A., Albayram, O., Draffehn, A., Michel, K., Piyanova, A., Oppenheimer, H., Dvir-Ginzberg, M., Rácz, I., Ulas, T., Imbeault, S., Bab, I., Schultze, J. L., & Zimmer, A. (2017). A chronic low dose of Δ9-tetrahydrocannabinol (THC) restores cognitive function in old mice. Nature medicine, 23(6), 782–787.
[9] Komorowska-Müller, J. A., Gellner, A. K., Ravichandran, K. A., Bilkei-Gorzo, A., Zimmer, A., & Stein, V. (2023). Chronic low-dose Δ9-tetrahydrocannabinol (THC) treatment stabilizes dendritic spines in 18-month-old mice. Scientific reports, 13(1), 1390.
[10] Sarne, Y., Toledano, R., Rachmany, L., Sasson, E., & Doron, R. (2018). Reversal of age-related cognitive impairments in mice by an extremely low dose of tetrahydrocannabinol. Neurobiology of aging, 61, 177–186.
[11] Fihurka, O., Hong, Y., Yan, J., Brown, B., Lin, X., Shen, N., Wang, Y., Zhao, H., Gordon, M. N., Morgan, D., Zhou, Q., Chang, P., & Cao, C. (2022). The Memory Benefit to Aged APP/PS1 Mice from Long-Term Intranasal Treatment of Low-Dose THC. International journal of molecular sciences, 23(8), 4253.
[12] Nidadavolu, P., Bilkei-Gorzo, A., Krämer, M., Schürmann, B., Palmisano, M., Beins, E. C., Madea, B., & Zimmer, A. (2021). Efficacy of Δ9 -Tetrahydrocannabinol (THC) Alone or in Combination With a 1:1 Ratio of Cannabidiol (CBD) in Reversing the Spatial Learning Deficits in Old Mice. Frontiers in aging neuroscience, 13, 718850.
[13] Meier, M. H., Caspi, A., Ambler, A., Hariri, A. R., Harrington, H., Hogan, S., Houts, R., Knodt, A. R., Ramrakha, S., Richmond-Rakerd, L. S., Poulton, R., & Moffitt, T. E. (2022). Preparedness for healthy ageing and polysubstance use in long-term cannabis users: a population-representative longitudinal study. The lancet. Healthy longevity, 3(10), e703–e714.
[14] Thayer, R. E., YorkWilliams, S. L., Hutchison, K. E., & Bryan, A. D. (2019). Preliminary results from a pilot study examining brain structure in older adult cannabis users and nonusers. Psychiatry research. Neuroimaging, 285, 58–63.
[15] Burggren, A. C., Siddarth, P., Mahmood, Z., London, E. D., Harrison, T. M., Merrill, D. A., Small, G. W., & Bookheimer, S. Y. (2018). Subregional Hippocampal Thickness Abnormalities in Older Adults with a History of Heavy Cannabis Use. Cannabis and cannabinoid research, 3(1), 242–251.
[16] Auer, R., Vittinghoff, E., Yaffe, K., Künzi, A., Kertesz, S. G., Levine, D. A., Albanese, E., Whitmer, R. A., Jacobs, D. R., Jr, Sidney, S., Glymour, M. M., & Pletcher, M. J. (2016). Association Between Lifetime Marijuana Use and Cognitive Function in Middle Age: The Coronary Artery Risk Development in Young Adults (CARDIA) Study. JAMA internal medicine, 176(3), 352–361.
[17] Watson, K. K., Bryan, A. D., Thayer, R. E., Ellingson, J. M., Skrzynski, C. J., & Hutchison, K. E. (2022). Cannabis Use and Resting State Functional Connectivity in the Aging Brain. Frontiers in aging neuroscience, 14, 804890.
[18] Stypulkowski, K., & Thayer, R. E. (2022). Long-Term Recreational Cannabis Use Is Associated With Lower Executive Function and Processing Speed in a Pilot Sample of Older Adults. Journal of geriatric psychiatry and neurology, 35(5), 740–746.
[19] Tumati, S., Lanctôt, K. L., Wang, R., Li, A., Davis, A., & Herrmann, N. (2022). Medical Cannabis Use Among Older Adults in Canada: Self-Reported Data on Types and Amount Used, and Perceived Effects. Drugs & aging, 39(2), 153–163.