A Core Senescence Biomarker Fights Inflammation
Researchers publishing in Nature Communications have found that p53, a biomarker and inducer of senescence, suppresses both inflammation and DNA damage in senescent cells.
Senescence against cancer
Read More
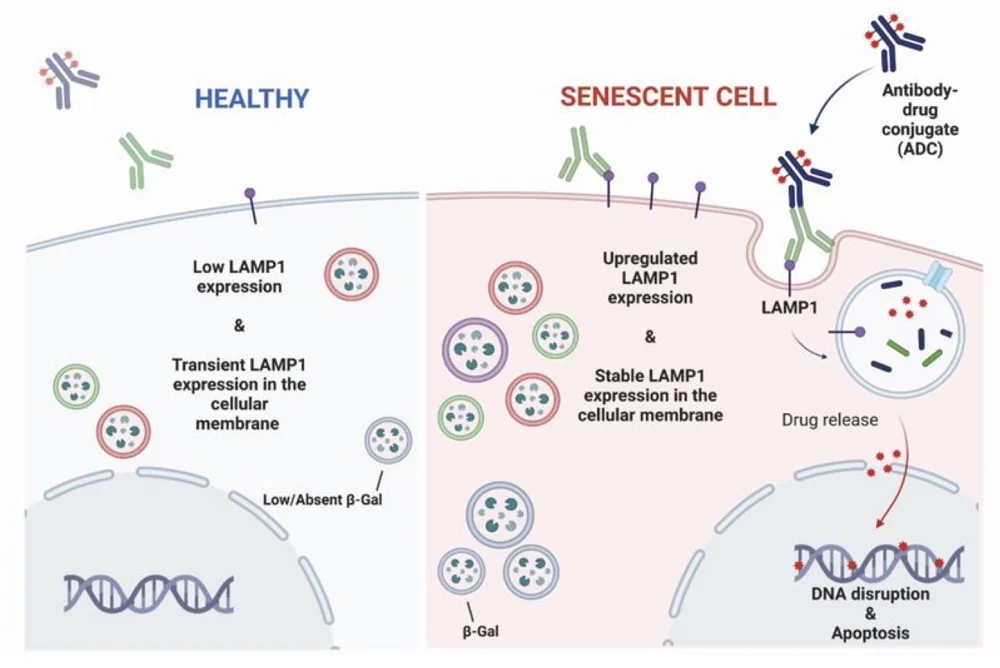
One of the main reasons why cells become senescent is to prevent cancer. The senescence-inducing compound p53, in particular, is known in the literature as a tumor suppressor, and its presence has been found to reduce, rather than exacerbate, the SASP [1]. The biochemical reasons behind this seemingly contradictory connection have not been previously explained.
However, these researchers have previously found that a biochemical pathway from the mitochondria to the nucleus is partially responsible for driving the SASP [2]. This pathway drives the expulsion of chromatin from the nucleus into the rest of the cell, which activates the cGAS/STING pathway and thus turns on NF-κB, the SASP’s master regulator [3]. Therefore, they sought to determine a link between p53 and this well-established pathway.
Preventing the SASP at its root
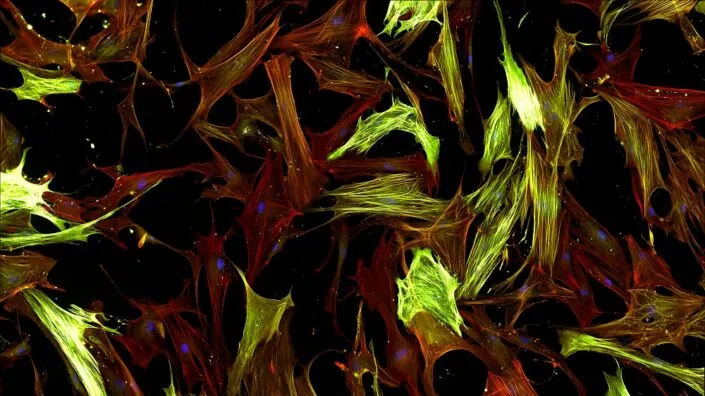
For their first experiment, the researchers created fibroblasts in which 53BP1, a suppressor of DNA damage that works with p53, was somewhat increased. These fibroblasts, after they were driven senescent through irradiation, had reduced amounts of chromatin in the nucleus and, thus, less SASP. Driving cells senescent by introducing p53 had similar effects, as did knocking down its target, MDM2.
Mutating 53BP1, on the other hand, had significant negative effects, spurring the release of chromatin into the nucleus after the cells were driven senescent with radiation. Silencing p53 had similar effects; four days after irradiation, cells with silenced p53 had significantly more chromatin in the nucleus. Further work found that mitochondria are required for this SASP upregulation; ablating away mitochondria prevented the chromatin from being expelled into the nucleus and thus prevented the upregulation of SASP elements.
Protecting cells from DNA damage
p53 was also found to be instrumental in DNA repair. γH2AX is a marker of DNA damage, and its levels in the nucleus were reduced in cells where MDM2 was downregulated and p53 was upregulated. The researchers found that this could be accomplished by introducing RG7388, a compound that promotes p53.
Similarly, silencing p53 increased the prevalence of this DNA damage marker. Interestingly, p21, another well-known biomarker of senescence, was found to be necessary for the effects of p53; without p21 being present, neither MDM2 nor p53 made any difference.
This was not just a change in a biomarker; p53 had real effects on the genome. In cells treated with RG7388 shortly after irradiation, the number of DNA amplifications and deletions was relatively small. In untreated cells, however, these signs of genetic damage were rampant. Most of this damage was located near the ends of the chromosomes, where the telomeres are. Unlike with chromatin ejection, however, mitochondria had nothing to do with these DNA damage effects.
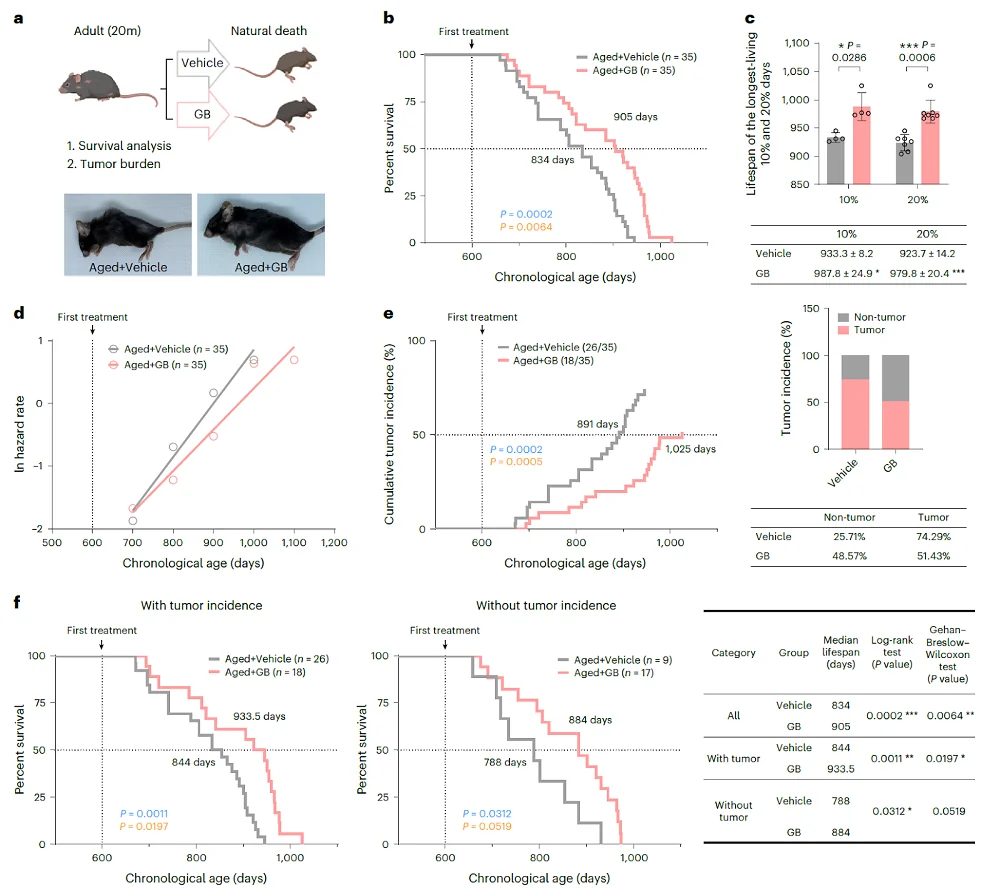
Effects in female mice
The researchers then turned to in vivo experiments, introducing HDM201, a compound that suppresses MDM2, to a population of naturally aged mice for two weeks. In both males and females, HDM201 had no effects on body weight, blood cell counts, or liver pathological biomarkers. However, as the liver is where senescent cells normally accumulate in mice [4], the researchers focused their attentions there. Both p53 and p21 were significantly increased in these mice.
Interestingly, in gene expression, this treatment had substantially greater effects on female mice than on male mice. While it had no senolytic effects, it reversed many of the gene expression changes caused by aging. As expected, many of these genes were related to the SASP, and, likewise, the number of immune cells that infiltrated into these mice’s livers was decreased as well.
Both p53 and p21 have been investigated in the context of senescence, with previous researchers considering them as potential targets to be suppressed. This work, however, demonstrates that these compounds are both necessary and beneficial for preventing senescent cells from getting out of control. The researchers describe p53 as a senomorphic compound; while it clearly does not remove senescent cells, it significantly blunts their negative effects on the cells around them. They hold that “it may be possible to one day design a treatment that targets p53 to promote healthier aging.”
Literature
[1] Coppé, J. P., Patil, C. K., Rodier, F., Sun, Y. U., Muñoz, D. P., Goldstein, J., … & Campisi, J. (2008). Senescence-associated secretory phenotypes reveal cell-nonautonomous functions of oncogenic RAS and the p53 tumor suppressor. PLoS biology, 6(12), e301.
[2] Vizioli, M. G., Liu, T., Miller, K. N., Robertson, N. A., Gilroy, K., Lagnado, A. B., … & Adams, P. D. (2020). Mitochondria-to-nucleus retrograde signaling drives formation of cytoplasmic chromatin and inflammation in senescence. Genes & development, 34(5-6), 428-445.
[3] Dou, Z., Ghosh, K., Vizioli, M. G., Zhu, J., Sen, P., Wangensteen, K. J., … & Berger, S. L. (2017). Cytoplasmic chromatin triggers inflammation in senescence and cancer. Nature, 550(7676), 402-406.
[4] Ogrodnik, M., Miwa, S., Tchkonia, T., Tiniakos, D., Wilson, C. L., Lahat, A., … & Jurk, D. (2017). Cellular senescence drives age-dependent hepatic steatosis. Nature communications, 8(1), 15691.