Michael Levin on Bioelectricity in Development and Aging
Michael Levin, professor at Tufts University and director of Allen Discovery Center, has been working for years on how bioelectrical patterns affect development and aging. His research proves that this often-overlooked part of biology is immensely important and that mastering its mechanisms might one day do wonders for human health and longevity. By manipulating ion channels in cells other than neurons, Levin’s team has been able to engineer growth of new limbs and organs, suppress cancer, and produce something that looks like entirely new forms of life. However, this research also touches on some deeply philosophical questions.
You started your career as a software engineer. How did you end up doing biology?
I was interested in biology from an early age, along with electrical engineering. As a child, I had asthma, and we didn’t have any medications [Michael’s family emigrated to the US from Russia when he was a child]. So, my dad used to take the back off of the TV set—we had this giant wooden thing with a tiny screen in the front and vacuum tubes in the back—and we would sit there and look at it as a way to distract me during attacks. I was absolutely fascinated that somebody knew how to put all that stuff together in just the right order to make the show come out on the other side. I remember asking my dad, “How did somebody know to do this?” and hhe said, “Well, you can learn to do this. It’s called engineering,” and I thought, “There you go. That’s the best magic.”
Then, I had an older friend who was into insects, bugs, and beetles. We would go outside and look at all this stuff, and he would point out that this is the egg that turns into a caterpillar that turns into a butterfly. I was always interested in those things, watching them develop and interact with each other and their environment.
When I came to the US, I discovered computers and realized that software was fascinating. Before college, I worked in scientific computing, writing code for companies and scientists, and wanted to work in AI, but having observed the state of computer science once I got to college, it became clear that we didn’t have any AI, and it wasn’t going to happen without learning about the one obvious case we do know: biology, where you watch right in front of your eyes a little blob of chemistry and physics become a creature with a mind, preferences, goals, and behavioral competencies.
So, I finished two BS degrees, one in computer science and one in biology, focusing on developmental biology. As I tell my students, there are two magical classes in the university. The first is developmental biology, where you see physics and chemistry becoming mind. The second is electrical engineering 101, where you start with Ohm’s Law and these very basic pieces of physics, and before you know it, you build something that does logic: the basic elements of thought.
How does your background affect your approach to biology?
Computer science and engineering really inform my thinking because they teach you to be comfortable with abstractions and coarse graining. Computer scientists are good at cutting biology’s endless complexity into chunks that matter, and we can say something useful without having to say absolutely everything. It’s like math, because it’s rigorous and allows you to explore the consequences of whatever ideas you can imagine, but it forces you to make things that actually run and work (the best parts of abstract thought and practical engineering).
You chose an area that’s not really popular with biologists, and not a lot of people are working in it. It’s actually amazing how few people are working in bioelectricity.
The reason I chose bioelectricity is that what I’m interested in fundamentally is how minds enter the physical world, how they scale, how they transform. If you think about what makes us greater than just a pile of neurons or cells in general, there must be some kind of cognitive glue. There must be policies that allow larger-scale systems to operate in spaces that their parts don’t operate in.
Which is what emergence is.
In neuroscience, we know what that is: electrophysiology enables this amazing network that underlies all these things that we do. I wanted to understand what the cognitive glue is for intelligence in other spaces. For example, the anatomical morphospace: development, regeneration, cancer suppression. All these things are not just a set of sequential chemical steps; they’re actually navigating a problem space.
One of the most amazing things about developmental and regenerative biology is the incredible plasticity and problem-solving capacity of groups of cells as they navigate that space. How is it that all the cells take that journey together? When you look at an embryo with hundreds of thousands or millions of cells, there’s alignment, the commitment of all the cells to the same story of where they’re going to in anatomical space.
I was very interested in understanding how that alignment happens, how an entire collective buys into the same story. In an important sense, models of the world, AKA stories, hold collectives together. All the cells are solving problems together because they’ve all bought into the same goal state they want to achieve.
To understand the physical mechanisms that enable a collective of cells to implement the same story, it turns out it’s exactly the same as in the brain. I was interested in this for a very long time, but for many years, I couldn’t say that. When you’re just starting out in such an unconventional area, you can’t tell people you’re studying cognition. The first grant proposal I wrote was, “I’m studying ion channel genes in development.” Reviewers said, ion channels are kind of weird, but genes in development makes sense, people study that, so okay.
After a while, having done some work on it, I was able to say, “Well, actually it’s voltage gradients in development.” Again, reviewers said that was pretty weird, but it followed from the prior work, so maybe it’s okay. After a while I could say, “No, it’s really computations in morphogenesis.” By now, I can say, “Actually, it’s cognition: decision making, memories, goal-directed problem solving.”
So, you’re studying cognition based on cells other than neurons, and you use an interesting definition of intelligence introduced by William James, which is basically the ability to get to a certain goal via different routes or means.
Yes, it’s a very nice definition because it’s very cybernetic. It doesn’t talk about brains, it doesn’t constrain what space a goal is in. It doesn’t say that you’re a brain or that you’re evolved or engineered. It’s a very generic definition that I think gets to the heart of what we mean by intelligence, which is the ability to adaptively navigate a problem space with some degree of competency to get your needs met.
Is this something that requires a certain level of algorithmic complexity?
That’s an interesting point. In some of the latest work on memories, I talk about this issue of a bow tie, like an hourglass turned on its side.
At any given moment, you don’t have access to the past. What you can access is the memory traces, the engrams that were left in your brain and body by things you did in the past. Your job is to continuously interpret those memory traces to build and update a model of what’s going on so that you can act in the future. It’s a model of continuous reinterpretation of your own memory traces.
I think the left side of that bow tie, the compression of experiences into the thin middle (the bow tie has this bottleneck, like an auto-encoder), that part is algorithmic. We can say how we do the compression, but the right side of that funnel, in my opinion, can’t be algorithmic. This is what is special about life, which is not the case with modern computer architectures.
The right side of that funnel has to be creative because you lost information going through that bottleneck. You cannot reinflate it algorithmically, meaning with steps that will get you exactly what you had at the beginning. What you can do, though, is have creative problem-solving: you get a prompt from your memories, and now you have this whole system for figuring out what that means for you.
I think the same thing is happening in anatomical space. The DNA you receive from past generations, we know it’s not a blueprint. I think of it as a prompt for a generative model. You receive these ‘memories,’ but now it’s up to you to interpret them. Under most circumstances, all things being equal, you will end up interpreting them the same way, which is why dogs have puppies and cats have kittens.
But we know that if you make some changes in their circumstances, the material is extremely clever at making other things. With a normal human genome, you could make an anthrobot as well as a human embryo. With a normal frog genome, you could make a xenobot as well as a frog embryo. With a planarian genome, you could make planarians with heads of other species. We’ve done this in our lab.
There’s a lot of interpretation going on; morphogenesis is a creative process. That’s important because the debate about whether some sort of computational analogy is a good tool for these kinds of things rages on. I think parts of it are algorithmic and parts of it are not algorithmic.
You mentioned a few important concepts that are part of your work: morphogenesis, planarian experiments, xenobots. The readers, at this point, might not know what all this means. So, can you briefly describe your research and where it currently stands?
One of the things we’re very interested in is that creative aspect of plasticity. This notion comes straight out of computer science, the idea of reprogrammability. Your genome tells every cell what computational materials it can have. Specifically, we’re most interested in ion channels and electrical synapses; the genome sets these materials for you.
This is already conceptually different from what many people are used to, which is that the genome is the software, right? But you’re introducing a different candidate, which is bioelectricity patterns. How does it work as software on top of the genetic hardware?
Hardware and software are, of course, a metaphor. The question is, “How do we apply this metaphor to biology?” The most popular way of mapping them is to say the genome is what matches the concept of software, and maybe the transcriptional machinery is the hardware. That’s the standard view.
I’m not saying it’s a bad metaphor; I’m saying it’s limited. There are scenarios where it prevents you from making novel discoveries. I’ll give you examples in bioelectricity, but there are other examples. There is also software that’s biochemical and runs on gene regulatory networks and chemical gradients. There’s also software that runs biomechanically on various physics gradients and forces. There are probably other things like biophotons.
I think bioelectricity makes the strongest case for this. There are numerous examples—we’ve developed a whole bunch of them—where knowing the genetic information leads you astray. It doesn’t tell you what’s actually going on.
For example, frog tadpoles don’t have legs, while axolotl embryos do have legs. We know their genomes. Now, in my lab, I make a “frogolotl.” A frogolotl is partly frog, partly axolotl. Looking at their genomes, can you tell me if a frogolotl is going to have legs or not? There’s no way to know. If it does have legs, will those legs contain frog cells or only axolotl cells? No models make predictions on this yet. Knowing the genetics is not enough to tell you what the pattern will be.
So, when it comes to developmental patterns, the genetics cannot really explain how an organism develops into its final form, how this type of intercellular communication works.
The genetics will certainly help you with the hardware of the communication. It will tell you that these cells have certain ion channels, certain ways to secrete chemical signals, gap junctions or synapses. What it doesn’t tell you is how the decision-making is going to work.
When a frog cell finds itself next to an axolotl cell, and all the axolotl cells are saying “build the leg” and the frog cells are not expecting to build a leg, what happens then? That’s a software question. You don’t get there from knowing the hardware.
Similarly, if I take two species of planaria (flatworms) with different shaped heads, and I take stem cells from one shape, stick them into the body of the other, and then cut the head off, what head shape is it going to make? Is one going to be dominant? Is it going to be an intermediate shape? Is it never going to stop regenerating because neither set of cells is ever happy about what’s happening?
These are questions that require understanding the decision-making of a collective intelligence: the group of cells that are navigating anatomical space. That’s very much a software question.
In our lab, we’ve studied examples where the software is a very important target for reprogramming the outcome. That’s critical because you can have philosophical debates about what’s software and what’s hardware, but the only reason any of that matters is: given however you’re using your metaphor, what does it enable you to do that couldn’t be done before?
Let me give you a few examples. We’ve shown that when you cut a normal planarian flatworm into pieces, every piece always develops one head, one tail. You can ask, how does it know how many heads it’s supposed to have? The standard answer is, “Well, the genome, of course.” Even though we know the genome doesn’t actually say anything about heads or head size or shape or number.
We developed the first molecular tools to read and write electrical information in living tissue, outside the brain. We’ve decoded bioelectrical patterns to understand how they say, “One head, one tail.” Then we said, “Let’s change the pattern so that it says, ‘two heads.'”
We don’t apply fields, there are no electrodes, frequencies, magnets, electromagnetic waves, nothing like that. We manipulate ion channels and gap junctions because that’s the electrical interface that the cells use to manipulate each other. So, we use ion channel drugs to manipulate the voltage pattern so that it says, “Two heads.”
If you do that, that fragment will regenerate with two heads. Not only that, but if you continue to cut that fragment in the future as many times as you want, with no more drugs of any kind, just regular water, they will continue generating two-headed worms forever. So now you have a strain of worms that has one head and a strain of worms that has two heads. The difference is not genetic; we didn’t touch the genome. There’s nothing genetically wrong with them. If you sequence them, you are none the wiser about why they have two heads.
So where does it say how many heads the worm should have? What the genetics actually gives you is a hardware specification that by default acquires a pattern that says, “One head”. Just like when you buy a programmable calculator from the store, when you turn it on, it says zero by default, but it’s reprogrammable, and living tissue is reprogrammable too. If you change the pattern it holds, it has a memory, and once you’ve set it to “two heads,” it holds.
Another example we have is in cancer, where we can introduce nasty human oncogenes into tadpoles, and they develop tumors. If we manage the voltage appropriately, you don’t get tumors even though the oncoprotein is still blazingly expressed.
We don’t kill the cells, we don’t fix the DNA, we don’t do anything with the DNA itself. Some hardware problems are fixable in software. In other words, you still have the oncoprotein, but if we keep that cell connected to the electrical network, then the collective works on nice things like building healthy skin or muscle, instead of being a unicellular organism and doing metastasis.
Your insights into cancer are very interesting: you say that it’s a cell reverting to its local unicellular goals, sort of losing communications with other cells.
I describe cancer as a dissociative identity disorder, quite literally. The right question is not “Why is there cancer?” It’s “Why is there anything but cancer all the time?”
Individual cells are very competent; they used to be unicellular organisms. But, how do you convince a bunch of cells to work together toward building this larger organism? Everything they do is focused on establishing metabolic, physiological, and other kinds of goals in a tiny 10-micron radius. That’s their size. I call this the “cognitive light cone”: it’s the size of the biggest goal you can work toward.
Individual cells have a quite small cognitive light cone; they pursue tiny local pH and metabolic states. But, you have this amazing thing in evolution and development where you suddenly pull cells together into a large network where the network has grandiose goals.
For example, in a salamander, the cells of the leg have the goal of building a leg. Why do I call it a goal? Because if I deviate them from that goal by cutting off the leg, they will spring into action, rebuild the leg, and then stop when it’s done. That’s the definition of a goal: it’s a cybernetic thing.
How did this happen? How is it that a bunch of cells together now have this giant cognitive light cone that’s centimeters in size and projects into a new space? Whereas before, it was projecting in physiological and metabolic space, now their goal exists in this anatomical space that individual cells don’t have access to.
What happened is that the cells are connected into a network that enables them to remember very large goal states.
Basically, a society of cells.
It’s a society, but it’s more than that. Any homeostatic process has to store the set point. There has to be somewhere where the set point is stored. In your thermostat, what you need to know is how to change the set point. Once you change it, the whole thing will act toward the new set point, no matter how the rest of it works.
Remembering what a salamander limb looks like is too much for one cell. Individual cells don’t know what a finger is or how many fingers you’re supposed to have, but groups of cells can, because they’re a larger computational network.
They’re a society, yes, but specifically they form a larger-scale processing network that can store these enormous goal states. That process builds larger intelligences that project with bigger cognitive light cones into new problem spaces.
That process obviously has a failure mode. What happens when cells disconnect from that electrical network? They can no longer remember that large goal. They revert back to their unicellular tiny little goals.
Before, the whole organism was “me,” and now the rest of the body is just the external environment. “I’m a single cell, but this external world—I don’t care what happens to it. I’m going to do whatever’s good for me.” That’s metastasis: “I’m going to replicate as much as I can, go where I want, eat what I want.”
If you have this view, you can approach cancer differently. Instead of killing the cells or trying to fix the genomics, you can forcibly reconnect them together. That’s what we’ve done, and it’s a therapeutic modality. We’re now moving from frogs to human tissues.
How is this information stored in that single cell where it all begins?
We can see how it’s stored: in the electrical circuits that are formed when the cell starts dividing. The really weird question is, where does the information come from? We have to dive into the philosophical question of what it means for something to come from somewhere.
Typically, biologists like information that comes either from history—meaning evolution or some kind of past events guided and made sure that the pattern was this and not something else. So, there’s a historical set of selection forces that made sure this is the information that’s here.
The other source is physics. In this case, both of those things are present. The history of evolution made sure that your cell has certain ion channels. By having certain ion channels, the excitable medium that you make when you have a collection of cells has certain properties. The electrical circuit has certain properties of memory, plasticity, symmetry breaking, amplification, and those processes are in part derived from the properties of the ion channels that are there. So, evolution is plugged in here.
Physics is absolutely also plugged in because some aspects of how electric circuits function are not part of biology; they’re part of physics and the laws of computation.
There’s a third component here. A similar problem has been discussed with respect to chemical patterns. Alan Turing, one of my heroes, was very interested in intelligence and unfamiliar embodiments. He wrote this paper on chemical self-organization and embryogenesis, weird for a guy interested in math, computers, and intelligence.
I think he saw a profound truth, and if he had lived longer, he would’ve written about it: the formation of the body and the formation of a mind are parallel, symmetrical processes. I think he was trying to get at this question of where the goal patterns of novel beings come from.
Typically, when you look at a goal-directed system such as any biological system, and you want to know why it makes the shape it makes or has the behavior it has, the answer is “Oh, evolution” because eons of selection made sure that’s what it has. But when you make new things, new bodies and new minds, as in AI or swarm robotics or any kind of collective intelligence, where do their goals come from?
When we make synthetic beings, such as xenobots and anthrobots (which are synthetic life forms made of cells), they’ve never existed before. There is no history of selection that makes for a good xenobot or tells an anthrobot what it has to be.
A xenobot, just to explain this to the readers, is sort of a clump of frog cells that begins its own life.
It’s what happens when you liberate some frog prospective skin cells from the embryo and take them away from the other cells that normally bully them into having a boring two-dimensional life as the outside of the embryo. Now, they get their own life, and they do something completely different. They organize into a little self-motile construct that runs around and does all sorts of interesting things, including reacting to sound stimuli.
They also reproduce, which I find pretty amazing.
It’s crazy. They do this kinematic self-replication. If you give them a bunch of loose epithelial cells, they will make more xenobots out of those. Then we do anthrobots, which are the same thing made out of adult human tracheal epithelial cells. We have a protocol that lets them assemble into this self-motile thing that does interesting things like heal neural wounds by joining them across the gap.
So there’s the history of selection, there’s stuff from physics, and the third thing is what Turing studied in his model of chemical symmetry breaking and amplification, reaction-diffusion systems and things like that. You have two chemicals that interact with each other in some particular way, and they make spirals or spots such as on a leopard, or stripes on a zebra.
Where do those patterns come from? There are two ways to address that question. One thing you can say is they’re emergent from the physical properties of the two chemicals that you have. You can say that, but it doesn’t really say anything. What emergence really says is “we got surprised.” We had things that we knew, we put them together, and then we got some new thing that we didn’t see coming.
I don’t like that because it feels like stamp collecting we’re just going to be surprised when we are, and we’ll write it down in our big book of emergent amazing things. What I like more is how many mathematicians look at it: there is an ordered, structured space of mathematical truths, like the Platonic space. Pythagoras also saw this very clearly—there is an ordered space of truths that matter functionally in the physical world.
Evolution makes use of them. They provide all kinds of “free lunches” for evolution. They make a difference in the physical world, but the key is that they themselves are not set by any facts of physics.
For example, if we look at a fractal, like these Halley plots, these amazing, beautiful, very organic-looking fractals that come from a very small formula, if you ask, “Where does that shape come from?” there are no facts of physics that determine it.
It emerges from a set of simple rules.
Basically, it’s a very simple rule, a very simple procedure that reveals this thing. When you want to ask where it comes from, you have two choices. You can say there’s a space of these patterns, and what you found is a pointer into that space. For a computer scientist, this looks exactly like pointers into a preexisting space of patterns.
When we make an embryo or a biobot or any kind of living or engineered thing, we’re providing a bunch of pointers or interfaces into that space of patterns. I like to assume, and this is a metaphysical stance, that it’s a structured, ordered space so that we can study it.
To me, Xenobots and Anthrobots are vehicles for studying the contents of that latent space. I don’t think that emergence as just “the surprising thing that sometimes happens” helps us enough. I think we have to assume it’s an ordered space. We have to make more tools to study it.
There are mathematical structures that will ingress into the physical world and guide what happens when you provide an appropriate interface. What’s an appropriate interface? If you want to see some basic facts around simple machines, you can make a lever and a fulcrum, and then you’ll see those patterns. If you want to see some facts of computation, you can make a bioelectric medium, and then you will see some of these patterns come through.
When we ask where these patterns come from, I think there are three factors: the two that are standard biology fare, evolution and physics, and then there’s this third thing, which I take very seriously, this space of patterns that we are now able to investigate systematically.
Rarely do I get to discuss the Platonic heaven with a geroscientist, but how is your research related to aging and age-related diseases?
The bare fact of the existence of planarians, I’m talking about the asexual forms that we have, is telling us that it is not the case that inevitably you accumulate mutations and get old and die.
Right, they’re one of the non-aging species, basically immortal.
Yes, the asexual planarians are immortal. So, we know that these ‘inevitable’ thermodynamic theories of aging cannot be the full explanation. Planarians give me hope that aging can be defeated.
Also, because planarians reproduce by asexual fission, they accumulate somatic mutations, and their genomes are a total mess. So, the fact that the animal with the messiest genome is also highly regenerative, cancer-resistant, and immortal also tells us that all this focus on genetics is somewhat misplaced.
After 20 years of driving myself crazy about it, I think we finally understand why there are no abnormal genetic strains of planaria. You can get flies with red eyes and crooked wings, and you can get mice with weird toes, but there are no weird kinds of planaria except for the two-headed strains that we made, and ours are not genetic. There’s a deep reason for that: planaria basically ignore most of their genetic information.
In planaria, individual cells die all the time and need to be replaced. When new cells come in, if you don’t know where to place them, you’re going to degrade over time. So, the ship of Theseus that is our body, the ship of Theseus isn’t the boat, it’s the plan in the mind of the workers who fix up the ship.
The collective must have a memory of what our body looks like so that it can continuously maintain anatomical homeostasis: that’s how regeneration works and how aging is resisted.
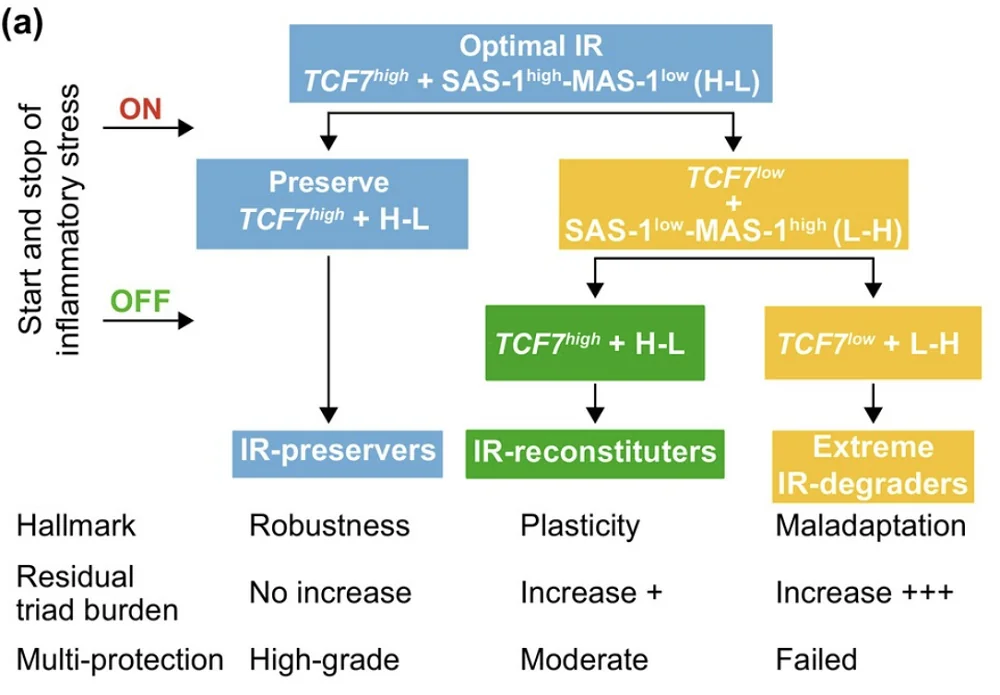
We study in our lab what happens to the bioelectrical pattern during aging. Two things can happen. First, the pattern can get degraded over time. If the bioelectrical pattern gets degraded, everything else is going to go wrong afterward.
We know this from our work in birth defects. We’ve shown that whether caused by chemical teratogens or by mutations in important genes, we can rescue terrible birth defects by forcing the appropriate bioelectrical pattern. If the bioelectrical pattern is good, it covers up a lot of defects in the hardware.
So, one possibility is that the bioelectrical pattern is getting fuzzy, and we’re now studying this. We have evidence for this in humans with senescent cells. The other possibility, of course, is that over time, the cells might become less able to execute the pattern; we have evidence for that too.
The first aspect is the bioelectric part of it, and how that relates to the goal of keeping the body plan implemented. Then there are two other things about aging that I think are quite different.
One is a cognitive theory of aging. The standard theories focus on whether it’s a thermodynamic noise issue or programmatic theories of aging where there’s an evolutionary reason we age and there are genes for this. But, there’s another option: what happens, given that the body is a goal-seeking agent that works to implement a certain anatomical goal in morpho-space, when that goal-seeking cognitive system has finished making its goal?
Think about the Judeo-Christian concept of heaven. You and your pet snake go to heaven, everything’s great. There is no noise, no degradation, no radiation, nothing. Everything’s perfect physically, for an infinity of years.
It’s like “happily ever after.” I’ve always asked myself this question too; it seems lazy as a concept.
Well, the question is: the snake maybe will be fine doing snake things every day, but for the human, do you really think we could stay sane? You’ll keep yourself busy for the first 10,000 years. What about after a billion years?
We did simulations of a goal-seeking morphogenetic system that was given a goal to build a body. It does, but then there is no new goal. What we observe, which is quite amazing, is that in the absence of noise and external stimulation, you have a fundamentally cognitive problem, which is dissociation. The pattern starts to degrade.
During embryogenesis, the goal gets met. Then, for some amount of time, there’s stasis, and then this thing just starts to degrade. We think that’s part of aging; what you need to do is either reinforce the goal or provide new goals. By new goals, I mean it’s possible that you’re not going to do a thousand years in the standard human body, but you could if every so often you switched it up a little bit, made some changes.
I think this is what planarians do when they split. The reason these asexual planarians are immortal is that every so often they provide a new challenge to themselves: they tear themselves in half, and that reminds all the cells what the morphogenetic goal is, and they rebuild. That gives them another few weeks to hang around, and then they do it again.
This kind of “boredom theory of aging,” that it’s fundamentally a cognitive dissociation at the bottom of it, is another thing we’re studying. The question is: can we use our bioelectric interface to provide a reminder to the cells of what they should be doing?
The third thing Leo Lopez in my group did was use phylostratigraphy, which is a bioinformatics tool that looks at gene expression and tries to estimate the age of various genes: “On the phylogenetic tree, how far back did these things appear?”
When he looks at transcriptomics from young humans and old humans, he finds something very interesting. As you get older, two things happen. First, some tissues start to differentially express genes that are further back on the phylogenetic tree. Not all tissues do this, but some do. They start to up- and downregulate more and more ancient genes. There’s this old observation that embryonic stages of development look like stages of evolution.
Where embryos of all kinds of species look like each other, and then they start to diverge.
Exactly. Very much like development traverses embryonic stages of past lineages, it looks like aging goes in the opposite direction. The cells start focusing on genes that are further and further back in evolution. Not only that, but you get this crazy dissociation where different tissues in the body do it quite differently.
When you’re young, all cells have a tight concordance of where you are on that phylogenetic tree, but when you get older, you start to get this divergence where the cells no longer agree as much.
One of the really wild possibilities is that whereas cancer is a kind of spatial dissociation, aging may be more of a temporal dissociation, floating off backwards on the scale of evolution. This gives rise to some of our efforts to remind cells what their priors are.
You have co-founded some interesting companies, including one working on regeneration in mammals.
There are three companies. Morphoceuticals works on using bioelectric cues to regenerate limbs. We did it in frogs some years ago, and we are now working on this in rodents. I don’t have anything to report yet; we’re still working on it.
Fauna Systems is formed around designing bespoke synthetic living machines for applications in the environment: sensing, cleanup. Right now, it’s mostly focused on xenobots, but there many other technologies are coming. The idea is using AI to help communicate novel goals to the materials so that you get biological robots of desired form and function.
The third company, which may be of the most relevance here, is called Astonishing Labs. It’s working on aging; all the stuff I told you today about aging are things that Astonishing Labs is doing. It’s also working on anthrobots, which are personalized in-the-body agential interventions. Anthrobots can be made of your own cells, so you don’t need immunosuppression.
If you had an infinite timeline, what do you think could be done with your work on bioelectricity for aging? What’s the best thing you can imagine?
Where I think this is going, assuming we all survive and live into the future to do science, I am looking at a world that has what I call “freedom of embodiment.” The children of the future will look back on this time (and it’s not that far off, I think we actually have a roadmap to it), and it’ll be like when we first learned about ancient humans, and we said, “My God, imagine living in a world where if you step on a sharp stick, you get sepsis and die.” The children of the future will look back at us and say, “You’re telling me that these people had to live in whatever body they were randomly given? And they had no choice about their IQ, capabilities, hopes and dreams?”
And, of course, lifespan.
Lifespan, diseases, and they were susceptible to all sorts of stupid viruses and bacteria, and they got lower back pain and astigmatism and brain degeneration, and everything was up to this random walk of evolution. Incredible. How could anybody live like this?
In the future, we’re going to have an “anatomical compiler” to specify what living form you want and compile it into a list of stimuli that have to be given to cells to get them to build what you want. At that point, forget about regeneration, aging, and injury. You will be able to have the body you want. You want an extra brain hemisphere? You want to directly sense the solar weather and the stock market? Why not? We’ve made them in the lab in model systems. Biology is incredibly plastic, and I absolutely think it’s possible.