
Your #1 Source for Life Extension News
Lifespan.io offers the latest information on rejuvenation biotechnology and life extension technologies. Our news outlet brings you the latest aging research, financial, and advocacy news, which is great if you like to keep up to date with everything happening in this rapidly changing field on a daily basis.
The Latest Longevity News Stories

The 2025 Longevity Summit Dublin
The 2025 Longevity Summit Dublin was held in July, and we have the highlights from the event for you along with the latest research updates and news from the conference. The Summit was founded by […]
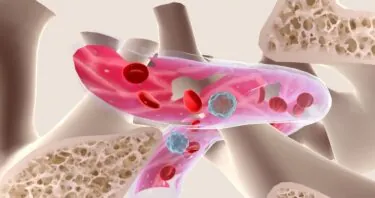
Non-Toxic Stem Cell Transplantation Prevents Cancer in Mice
Scientists have developed a protocol for hematopoietic stem cell transplantation that reconstructs a healthy blood system and prevents blood cancers in old mice while also reducing toxicity [1]. The blood factory […]
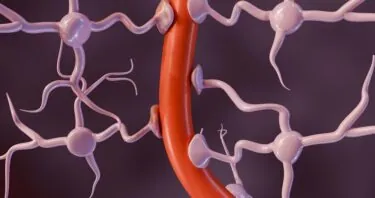
How Blood-Brain Barrier Leaks Make Parkinson’s Worse
Researchers have discovered how α-synuclein (α-syn), a key protein in Parkinson’s disease and Lewy body dementia, leads to inflammation and disruption of […]

Scientists Successfully Edit Mitochondrial DNA
A new study demonstrates that novel gene-editing tools can correct disease-causing mutations in mitochondrial DNA in primary human cells [1]. Smaller editing tools needed Genome-editing tools such as […]

Senolytics May Affect Inflammation-Related Cognitive Decline
Researchers have found that inflamed, senescent microglia prune too many synapses in the hippocampus and demonstrated that a senolytic compound can ameliorate this process in Aging Cell. Some synapse […]

Gabriel Cian on Investment and the 2060 Longevity Forum
In this Lifespan interview, we speak with Gabriel Cian, founder of the 2060 Longevity Forum, about how his background in software shaped his views on healthspan innovation, the forum’s approach […]

Molecular Similarities Between Cigarette Smoking and Aging
Researchers have analyzed molecular patterns from different tissues obtained from over 700 people and learned that smoking acts as an aging […]

Inflammaging Might Not Be Universal Across Populations
By comparing data from industrialized and non-industrialized societies, a new study calls into question some assumptions about the relationship between inflammation and aging [1]. Harmful protection Inflammation accompanies us throughout our entire lives. Without it, we […]

Five Hallmarks of Stem Cell Aging Proposed
In Cell Stem Cell, a trio of reviewers has proposed five hallmarks that are specific to the aging of stem cells. Functional rather than molecular This […]

Dr. David Furman on Inflammation and Aging
The longevity field hasn’t been very good at naming things, but one notable exception is “inflammaging”: the low-grade chronic inflammation that correlates with aging. Recognition has been growing that inflammation, the ubiquitous reaction […]

Fixing Sugar Metabolism Shows Promise Against Dementia
Scientists have shown that aberrant metabolism of glycogen in neurons is linked to the accumulation of harmful tau protein. Caloric restriction, genetic interventions, and small molecules might help [1]. Glycogen and […]

Researchers Connect Cellular Markers to Physical Well-Being
In Aging Cell, a team of researchers has described how the health of skin fibroblasts relates to physical and functional ability. Frailty, capacity, and skin cells This paper begins with an explanation of […]
Interviewing the leading experts in aging research and longevity
We have a dedicated team of journalists who have interviewed many of the leaders in the field about their research and the drive to end age-related diseases. You can find our latest interviews below.
Regular Digest Articles
We publish the Rejuvenation Roundup – a monthly digest of what is happening in the field, a Longevity Market Recap – a monthly digest focused on the investment and business side of the field, and a quarterly Editorial – focusing on the activities of the news outlet and the wider organization.
Industry Press Releases
You can find some press releases from various companies in our field below. Lifespan.io does not endorse any of these PRs and they are simply provided for information and interest.
Want even more news?
If you want to see even more recent articles, check out all news stories, or if you would like to look at a specific year or month head to the news archive.













