Vitamin K is not a single vitamin but a family of fat-soluble vitamins with a common core structure [1]. Members of this family can be divided into two groups: phylloquinone (Vitamin K1) and menaquinones (Vitamin K2). The entire family assists vitamin K-dependent carboxylase, which is an enzyme required to make proteins involved in blood clotting, bone metabolism, and other functions [2,3]. Despite this common function, K1 and K2 have different origins in nature and assume distinct roles in the body.
Two of the most notable members of the K2 family are MK-4 and MK-7. Here, MK stands for menaquinone, and the number refers to the length of a specific side chain in the molecule’s structure. While the longer side chain of MK-7 results in this molecule remaining in circulation for a longer period [4], their functions are similar.
Sources of K2
K2 is a product of bacterial fermentation, so fermented foods are major sources of K2 [1,2]. Small but significant amounts of K2 are produced by intestinal bacteria, although this amount varies due to individual microbiome differences [5].
Natto (a traditional Japanese food made from fermented soybeans) has considerable amounts of K2 [1,6]. The quantity of K2 in other fermented foods, such as soft cheese and sauerkraut, may vary according to the bacterial strains used in the fermentation. Animals can synthesize MK-4 from menadione, a synthetic form of vitamin K that is found in poultry and swine feed [7]. However, without knowing if menadione is added to their feed, these meats cannot be relied upon for their K2 content.
Interestingly, an analysis of microbiome gene expression revealed that Type 2 diabetics had an increase in K2 due to more K2-synthesizing bacteria [8].
Retailers sell K2 supplements as both MK-4 and MK-7. Although some studies have shown mixed results of these supplements for osteoporosis, evidence suggests that this is related to differences in the co-administration of Vitamin D and calcium to study participants [9].

[10,11]
K2 is a fat-soluble vitamin that regulates multiple processes in the human body through the activation of Vitamin K2-dependent proteins. Two of these proteins, matrix Gla and osteocalcin, play a prominent role in the function of the cardiovascular and skeletal systems [12]. In addition, through poorly understood mechanisms, K2 plays a significant role in the health of the digestive system, which can affect other bodily systems.
Ingested Vitamin K is integrated into microscopic lipid bubbles (micelles), which are absorbed by the small intestine, transported to the liver, and packaged into very low-density lipoproteins [2,13]. The body retains 30-40% of ingested Vitamin K2, but it is rapidly metabolized and excreted. Unlike other fat-soluble vitamins, Vitamin K2 does not remain in the body for extended periods. No data on normal ranges of K2 are available [2].
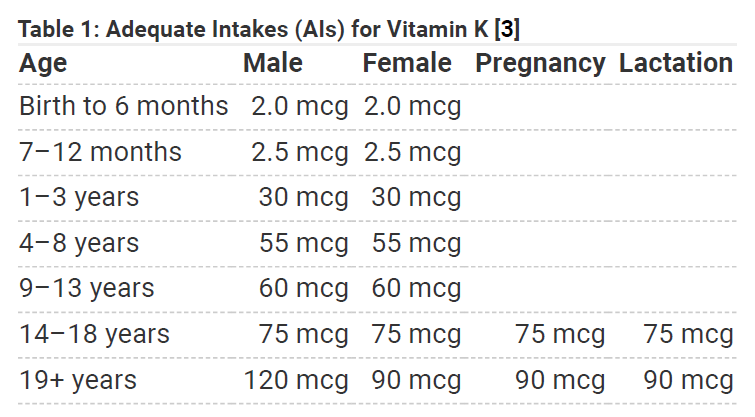
The Food and Nutrition Board has, however, established adequate intakes for males and females [14], but it does not appear that these values reflect recent findings associated with arterial calcification and osteoporosis. Numerous studies suggest higher dosages can protect against a host of bone, cardiovascular, and digestive diseases. Furthermore, no adverse effects are associated with high doses of K2 [14].
Interactions with pharmaceutical drugs
Vitamin K is known to interact with several medications, including warfarin and other anticoagulants, antibiotics, bile acid sequestrants, and orlistat. Anticoagulants antagonize the activity of Vitamin K and deplete K1 clotting factors. It would be reasonable to suspect that anticoagulants would have the same effect on K2, given that K1 and K2 have the same core chemical structure.
Vitamin K2 intakes
Most U.S. diets are said to contain adequate amounts of K, with intakes averaging 122 micrograms for women and 138 micrograms for men. When food and supplement use are factored together, the average K intake increases to 164 micrograms for women and 182 micrograms for men [5]. However, these studies did not look at the sources of Vitamin K, nor did they make any distinctions between the quantities of Vitamins K1 and K2. Given the differences in the sources from which these K variants are derived, the average K2 intake is not clear, but the consumption of K2-containing fermented foods is less popular in the United States and Europe than in other areas of the world, such as Asia.
Malabsorption disorders affect vitamin K
People with malabsorption syndromes and other gastrointestinal disorders, such as cystic fibrosis, celiac disease, ulcerative colitis, and short bowel syndrome, might not absorb Vitamin K properly [3,14,15].
Vitamin K and health
Cardiovascular health and K2
Arterial calcification is a major predictor of cardiovascular morbidity and mortality [16]. Matrix Gla protein (MGP) is a vitamin K-dependent protein that inhibits calcification of vascular and soft tissues [17].
Vascular calcification is caused by deposits of calcium phosphate, mostly in the form of hydroxyapatite. Hydroxyapatite is a major constituent of normal teeth and bones. Ninety percent of your tooth enamel and 60% of your bone is made from this mineral. It adds rigidity to your teeth and bone structure, repairs cavities, and regenerates teeth [18]. K2 helps ensure calcium phosphate goes to the right place.
Several factors, including high blood pressure, inflammation, oxidized LDL, stress, high calcium, and high phosphate, can cause vascular smooth muscle cells to resemble bone-producing cells. Individuals with diabetes, kidney problems, parathyroid issues, or atherosclerosis are particularly vulnerable to this process. The vascular smooth muscle cells of diabetics are exposed to extremely elevated levels of glucose, often for sustained periods. Non-animal experiments show that vascular smooth muscle cells, when exposed to high concentrations of glucose, proliferate rapidly and express bone-related proteins such as osteopontin [19].
Individuals with sluggish kidney function are unable to clear phosphorus from their systems as quickly as they need to. This results in elevations of serum phosphorus, which drives the formation of excess hydroxyapatite [20], thus hastening arterial calcification.
The parathyroid often becomes dysregulated because of poor kidney function, but it can do so independently. The parathyroid regulates serum calcium and phosphorus. In hyperparathyroidism, these minerals are elevated, thus increasing the risk of arterial calcification by driving the excess production of hydroxyapatite.
Lastly, atherosclerosis is initiated by mechanical or chemical injury to the innermost layer of the arteries. Injury causes the release of cytokines and initiates inflammatory processes, which produce a pro-calcification environment [21].
Bone health and K2
Osteoporosis affects more than 10 million U.S. adults, 80% of whom are women. Consuming enough calcium and Vitamin D throughout life is essential to maximize bone mass and reduce the risk of osteoporosis [22]. The effect of K2 intake on bone health and osteoporosis has recently been a focal point of research into this disease.
MGP and another K2-dependent protein, osteocalcin, both play a role in normal bone metabolism [12]. Osteocalcin is present in bone and is involved in bone mineralization or turnover [3]. Vitamin K2 is required to activate osteocalcin in bone, and vitamin K deficiency may result in reduced bone mineralization and contribute to osteoporosis [23].
A 2006 review examined trials that studied vitamin K supplementation on bone density and fractures in post-menopausal women. It showed that supplementation with MK-4 improved bone mineral density [24]. These trials used MK-4 at either 15 or 45 milligrams per day. Even at 1.5 milligrams per day, MK-4 supplementation significantly reduced fracture rates across the body [25]. A later clinical trial found that MK-7 supplementation at 180 micrograms per day, an even smaller dose, for three years improved bone strength and decreased the loss in vertebral height in postmenopausal women [26]. The fact that no adverse reactions were cited in the high-dose analysis is substantial evidence that this supplement is very safe at an effective dose.
However, other trials have found K supplementation to be less effective in elderly men and women [9]. In one study, 381 postmenopausal women received 45 milligrams of MK-4 or placebo daily for 12 months. All participants also received daily supplements containing 630 milligrams of calcium and 400 IU of vitamin D3. At the end of the study, participants receiving MK-4 had significantly lower levels of unactivated osteocalcin compared to those receiving placebo. However, there were no significant differences in bone mineral density of the lumbar spine or proximal femur among any of the treatment groups [9]. The administration of vitamin D and/or calcium along with vitamin K could partly explain why some studies have found that vitamin K supplementation improves bone health while others have not.
Immune function, endocrine health, and K2
Vitamin K2 at 60 micrograms and 100 micrograms inhibited T-cell proliferation in post-menopausal women. T-cell proliferation is often abnormally high in post-menopausal women [27].
T cells are thought to play a role in the development of postmenopausal bone loss, and this is believed to be controlled by estrogen and the immune system. The fact that mice deficient in T cells are protected from bone loss strengthens this argument [28].
MK-4 has been shown to enhance testosterone production in a dose-dependent manner in rats and testis-derived tumor cells. CYP11A, an enzyme that controls the production rate of different steroids such as testosterone, was stimulated by the presence of MK-4 [29].
Gut health and K2
K1 and K2 increase IAP through mechanisms that are not clear [30]. In addition, K2 stimulates bone ALP [31]. In this context, the increase in ALP is not associated with pathology.
K2 has been shown to activate the nuclear receptor pregnane X (PXR). This beneficially increases the expression of genes related to bile acid synthesis (necessary for digestion), glucose, and lipid control in mice with humanized PXR [32].
Literature
[1] S. L. Booth, “Vitamin K: food composition and dietary intakes,” Food & Nutr. Res., vol. 0, no. 0 SE-Vitamin Supplement, Apr. 2012
[2] S. J. Elder, D. B. Haytowitz, J. Howe, J. W. Peterson, and S. L. Booth, “Vitamin K Contents of Meat, Dairy, and Fast Food in the U.S. Diet,” J. Agric. Food Chem., vol. 54, no. 2, pp. 463–467, Jan. 2006
[3] P. M. Coates, M. R. Blackman, G. M. Cragg, M. Levine, J. Moss, and J. D. White, “Encyclopedia of dietary supplements,” Encycl. Diet. Suppl., pp. 1–821, 2004
[4] L. J. Schurgers, K. J. F. Teunissen, K. Hamulyák, M. H. J. Knapen, H. Vik, and C. Vermeer, “Vitamin K–containing dietary supplements: comparison of synthetic vitamin K1 and natto-derived menaquinone-7,” Blood, vol. 109, no. 8, pp. 3279–3283, 2007
[5] M. Serda et al., “Modern nutrition in health and disease: Eleventh edition,” Uniw. slaski, vol. 7, no. 1, pp. 343–354, 2012
[6] L. J. Schurgers and C. Vermeer, “Determination of phylloquinone and menaquinones in food. Effect of food matrix on circulating vitamin K concentrations,” Haemostasis, vol. 30, no. 6, pp. 298–307, 2000
[7] USFDA, “CFR – Code of Federal Regulations Title 21.”
[8] N. R. Dash and M. T. Al Bataineh, “Metagenomic Analysis of the Gut Microbiome Reveals Enrichment of Menaquinones (Vitamin K2) Pathway in Diabetes Mellitus,” dmj, vol. 45, no. 1, pp. 77–85, May 2020
[9] N. Binkley et al., “Vitamin K treatment reduces undercarboxylated osteocalcin but does not alter bone turnover, density, or geometry in healthy postmenopausal North American women,” J. Bone Miner. Res., vol. 24, no. 6, pp. 983–991, Jun. 2009
[10] InnovixLabs, “Foods that Contain Vitamin K2.”
[11] USDA National Nutrient Database for Standard Reference Release 28, “USDA National Nutrient Database for Standard Reference Release 28 Nutrients: Vitamin K2 ug,” Natl. Agricurtular Libr., vol. 4, pp. 1–236, 2016.
[12] L. J. Schurgers, “Vitamin K: key vitamin in controlling vascular calcification in chronic kidney disease,” Kidney Int., vol. 83, no. 5, pp. 782–784, 2013
[13] M. J. Shearer, X. Fu, and S. L. Booth, “Vitamin K Nutrition, Metabolism, and Requirements: Current Concepts and Future Research,” Adv. Nutr., vol. 3, no. 2, pp. 182–195, Mar. 2012
[14] P. Trumbo, A.A. Yates, S. Schlicker, M. Poos, “Dietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc,” J Am Diet Assoc. Mar; 101(3): 294-301, 2001
[15] V. A. Jagannath, Z. Fedorowicz, V. Thaker, and A. B. Chang, “Vitamin K supplementation for cystic fibrosis” , V. A. Jagannath, Ed. Chichester, UK: John Wiley & Sons, Ltd, Aug 22 8(8); CD008482 2017.
[16] M. Pluquet, S. Kamel, G. Choukroun, S. Liabeuf, and S. M. Laville, “Serum Calcification Propensity Represents a Good Biomarker of Vascular Calcification: A Systematic Review,” Toxins, vol. 14, no. 9. 2022
[17] R. Flore et al., “Something more to say about calcium homeostasis: the role of vitamin K2 in vascular calcification and osteoporosis,” Eur. Rev. Med. Pharmacol. Sci., vol. 17, pp. 2433–2440, Sep. 2013.
[18] E. Pepla, L. K. Besharat, G. Palaia, G. Tenore, and G. Migliau, “Nano-hydroxyapatite and its applications in preventive, restorative and regenerative dentistry: a review of literature,” Ann. Stomatol. (Roma)., vol. 5, no. 3, pp. 108–114, Nov. 2014
[19] N. X. Chen and S. M. Moe, “Arterial calcification in diabetes,” Curr. Diab. Rep., vol. 3, no. 1, pp. 28–32, 2003
[20] W. N. Suki and L. W. Moore, “Phosphorus Regulation in Chronic Kidney Disease,” Methodist Debakey Cardiovasc. J., vol. 12, no. 4 Suppl, pp. 6–9, 2016
[21] A. L. Durham, M. Y. Speer, M. Scatena, C. M. Giachelli, and C. M. Shanahan, “Role of smooth muscle cells in vascular calcification: implications in atherosclerosis and arterial stiffness,” Cardiovasc. Res., vol. 114, no. 4, pp. 590–600, Mar. 2018
[22] Office of Women’s Health, “Osteoporosis.”
[23] K. Maresz, “Proper Calcium Use: Vitamin K2 as a Promoter of Bone and Cardiovascular Health,” Integr. Med. (Encinitas)., vol. 14, no. 1, pp. 34–39, Feb. 2015
[24] S. Cockayne, J. Adamson, S. Lanham-New, M. J. Shearer, S. Gilbody, and D. J. Torgerson, “Vitamin K and the Prevention of Fractures: Systematic Review and Meta-analysis of Randomized Controlled Trials,” Arch. Intern. Med., vol. 166, no. 12, pp. 1256–1261, Jun. 2006
[25] N. Koitaya et al., “Low-dose vitamin K2 (MK-4) supplementation for 12 months improves bone metabolism and prevents forearm bone loss in postmenopausal Japanese women,” J. Bone Miner. Metab., vol. 32, no. 2, pp. 142–150, 2014
[26] M. H. J. Knapen, N. E. Drummen, E. Smit, C. Vermeer, and E. Theuwissen, “Three-year low-dose menaquinone-7 supplementation helps decrease bone loss in healthy postmenopausal women,” Osteoporos. Int., vol. 24, no. 9, pp. 2499–2507, 2013
[27] V. D. Myneni and E. Mezey, “Immunomodulatory effect of vitamin K2: Implications for bone health,” Oral Dis., vol. 24, no. 1–2, pp. 67–71, Mar. 2018
[28] S. L. Teitelbaum, “Postmenopausal osteoporosis, T cells, and immune dysfunction,” Proc. Natl. Acad. Sci. U. S. A., vol. 101, no. 48, pp. 16711–16712, Nov. 2004
[29] A. Ito et al., “Menaquinone-4 enhances testosterone production in rats and testis-derived tumor cells,” Lipids Health Dis., vol. 10, no. 1, p. 158, 2011
[30] N. Sogabe, R. Maruyama, T. Hosai, and M. Goseki-Sone, “Enhancement Effects of Vitamin K1 (Phylloquinone) or Vitamin K2 (Menaquinone-4) on Intestinal Alkaline Phosphatase Activity in Rats,” J. Nutr. Sci. Vitaminol. (Tokyo)., vol. 53, no. 3, pp. 219–224, 2007
[31] S. Akbari and A. A. Rasouli-Ghahroudi, “Vitamin K and Bone Metabolism: A Review of the Latest Evidence in Preclinical Studies,” Biomed Res. Int., vol. 2018, p. 4629383, Jun. 2018
[32] H. Sultana et al., “Effects of Vitamin K2 on the Expression of Genes Involved in Bile Acid Synthesis and Glucose Homeostasis in Mice with Humanized PXR,” Nutrients, vol. 10, no. 8, p. 982, Jul. 2018



