Joe Betts-Lacroix on Retro Bio and Its Recent AI Advancement
Retro Biosciences, one of the hottest startups in the longevity field, was founded about five years ago by the tech entrepreneur Joe Betts-Lacroix with a $180 million investment from his friend Sam Altman, the CEO of OpenAI. Despite its hefty war chest, the company initially pursued an image of an agile, scrappy company headquartered in refurbished containers. It also boldly went after several big ideas at once.
Since then, things have settled down a bit. Now, Retro has four major programs in development, three of which are related to cellular reprogramming. This explains the big news that made quite a splash last month, highlighting the company’s OpenAI roots: using a dedicated AI model based on GPT architecture, Retro scientists were able to tweak some of the existing reprogramming factors (or create new ones, depending on how they are defined), greatly improving reprogramming efficiency. We talked to Joe about this big announcement and other exciting Retro-related topics.
Your personal journey to the longevity field is one of the most interesting I’ve ever seen. I wanted to ask how you feel about fighting aging and extending human healthspan and lifespan, and what led you down this path.
I think in some latent way, as a technologist, there was a general draw toward the idea that there should be some way of interacting with the biology of how and why bodies fall apart. But based on my prior experience, it stayed latent because it didn’t seem to me like there was any tractable approach. Biology just seemed unimaginably complicated, and it felt like there was nothing to be done.
Any time there was a discussion or proponents of some way of improving health, there would be an equal number of people arguing the opposite, with no way to resolve the controversies. People were saying, “You should eat low-fat,” and other people were like, “No, you should eat low-sugar or low-protein.” If you followed everybody’s rules, you’d basically eat nothing.
Then I read a book somewhat randomly by an actual legit aging biologist, Roy Walford, who unfortunately is no longer with us. That was around 2008 or 2009. He opened my eyes to the fact that there are solid ways of collecting evidence about the effects of interventions on complex organisms like mammals and humans. In humans, you can actually separate the signal from the noise – where noise also includes lots of people claiming things – by doing randomized controlled clinical trials with placebos and prospective hypotheses.
That got me thinking, “Huh, there’s real science in here. There are interventions in experimental animals, which can be compared to humans on all these different physiological parallels, where small changes to the structure of the animal can make big changes in their lifespan.”
Then I was working for a while with the guys who ran Halcyon Molecular, and a bunch of them were also interested in aging biology. It was one of their deeper motivations for wanting to do better DNA sequencing. Whether you believe the argument for that is potent with respect to making a big difference in age-related disease, it just created more energy among a bunch of people for the topic.
It got to the point where I decided, “Wait, we should really do something as a society about this”. A couple of years after I read Walford, I decided to start a nonprofit foundation.
And this was a few years after you sold your company and tried to retire?
Yeah, I kind of experimented with, “What if I just chill forever now?” And then I was like, well, forever isn’t very long. It’s just silly to sit here while people are dying of age-related diseases, and maybe I should at least make some difference.
The main tangible step I could take at that time was to create a nonprofit foundation called the Health Extension Foundation and just start elevating the conversation in Silicon Valley, which is where I was hanging out. At that point, the public conversation was essentially people trying to sell vitamin creams and random, markety stuff that makes a dollar but didn’t have good evidence to support it.
I wanted to educate people in Silicon Valley because that’s where a lot of change comes from in the world, and they’re my people. So, I started creating this lecture series where I brought in PIs from the aging biology academic community to come give talks to a hundred or two hundred interested folks at a time. That’s where the momentum started for me.
Then there was the Y Combinator connection with Sam Altman, right?
There were actually two Y Combinator connections, in a sense. The first was right around the time I was reading Walford. I was part of this private tech hacker community, and I ran into a guy who brought a self-driving unicycle. I had commuted from Harvard to MIT on a unicycle because I was living in Harvard Square and doing grad school at MIT, and it was very portable and fun. So, I was naturally interested in it. This guy, Trevor Blackwell, had built a self-balancing one – at least it took care of the front-back axis.
We just hung out a bit. He was working on robots, and then I started this health extension thing and mentioned it to him. He said, “Why don’t you use Y Combinator as the space for holding these public events?” which I did for roughly the first half a year of the foundation. Then the events got too big for the YC space, so I started finding other spaces around the peninsula and in San Francisco to run them in every month. Later, Jared Friedman invited me to be a part-time partner there, and that’s how I ran into Sam.
Do you think Sam is also passionate about life extension, or was it just an investment for him?
He was definitely interested in entrepreneurs doing meaningful things in biology. While I was at YC, he, Matt Krisiloff, and I created an experimental program called YC Bio. We attempted to adapt the YC model to biology, which is slower – you can’t have a total revolution in three months. So, it had a longer time period to demo, more money, it took more equity in exchange for the more money, and it also provided lab space. Clearly, he was interested at that point.
After we both left YC, we often discussed potential bio ventures. Then after the sale of my second company, he was like, “Great, come to dinner!” It took a few months for me to find exactly which next company I wanted to start. What became Retro didn’t really get started from an operational perspective until 2021.
Let’s move to some recent events. You have your first trial scheduled for later this year, for a molecule that’s supposed to reverse Alzheimer’s disease by improving autophagy. Can you tell me about it?
Yes, it is an orally bioavailable small molecule that also happens to cross the blood-brain barrier. It restores the autophagy process that tends to get stuck in older cells that get overloaded with internal waste products.
It operates on a fairly general mechanism, and we’ve shown that it improves the proxy molecular markers of multiple accumulation-related diseases. We decided that we would start with familial Alzheimer’s disease. Even though I know it is a really big swing, we are also a relatively well-funded and adventurous biotech that can do things like that. So, we’re going for it.
Like many companies, you’re planning trials in Australia. Why has it become such a popular place?
There are so many great things about Australia, other than it being a long plane flight. The Australian government is fairly inspired in its intention to make Australia have a vibrant R&D ecosystem. One of the ways they do that is by incentivizing companies that do R&D there with a tax rebate. That provides the financial incentive to go there, which is the spark to check it out.
But then, once you actually start talking to the people who do R&D there, you find they have a very adventurous, can-do spirit. The regulatory environment is very efficient, especially for running early-stage trials with small molecules. It’s very smooth, no-nonsense, and practical. It feels more startup-friendly for human clinical research than Silicon Valley, ironically.
I believe three of your four candidates are based on cellular reprogramming. Has Retro effectively become a reprogramming company? Is this your biggest bet?
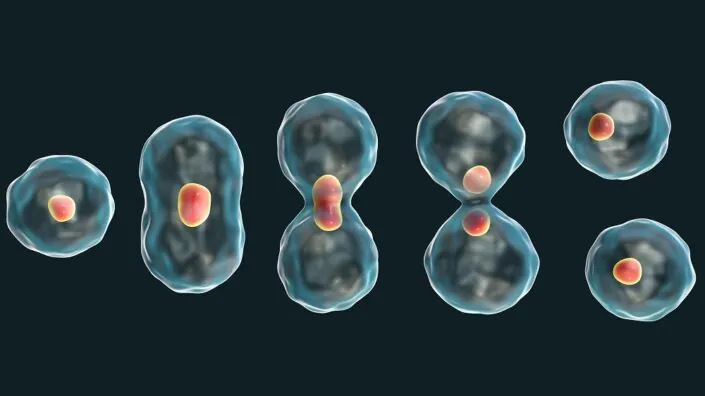
In one way or another, yes, we are for sure. We have a partial reprogramming research program that is not yet ready for clinical prime time, and then we have two clinical programs that use full reprogramming, which is exciting because it does essentially full rejuvenation, depending on the different ways of measuring the age of a cell. By most of those means, when you do full reprogramming all the way to an iPSC [induced pluripotent stem cell], you get essentially full rejuvenation.
What do you believe in more: the partial in vivo path or the full iPSC reprogramming in vitro path?
It’s hard to say what I’m most excited about. It’s like saying, “Which of my children do I love the most?” The problem with full reprogramming is that there are only a few cell types you can do it on. You need full control over the cell environment to differentiate it back to some adult cell type. So, a huge disadvantage is that you can’t do it in vivo. It pretty much only works for dissociated cells that are going to an individual cell type rather than a whole structured tissue. From an age-related disease intervention perspective, it can only work for cells that you can put back into the body as single cells.
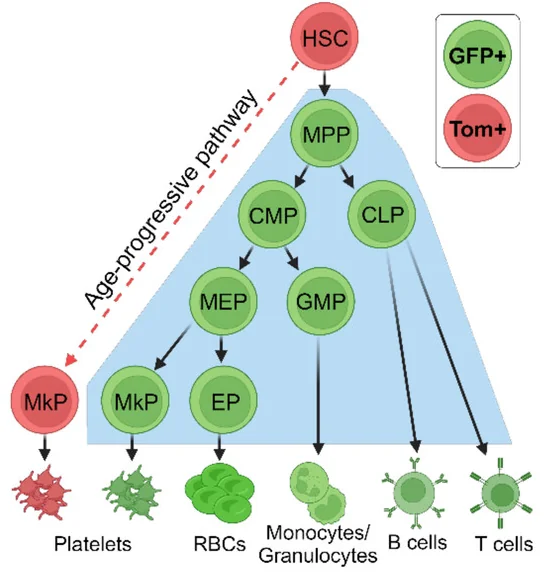
So that reduces the scope a lot. I am excited about it because I love the full rejuvenation and the ability to be reductionistic, controlling the entire environment step-by-step. But I wish there were more cell types that were amenable. Right now, we’re doing what we think are the two most viable and important ones, which are HSCs [hematopoietic stem cells] and microglia.
Fortunately, for HSCs, the healthcare community has gotten quite good at replacing the cells because of experience with leukemia, doing autologous bone marrow transplants for lymphoma or myeloma, or allogeneic transplants for various leukemias. It’s a well-developed path. But for the larger picture of the hundreds of cell types in other parts of the body, I think partial reprogramming is a huge opportunity. It’s just harder and more complicated.
Is that why you have that program on a back burner right now?
Yes, it’s operating outside of the clinical context. The moment we say, “Okay, time to go to the clinic,” that’s a very special mode for a program to go into. It requires a canonical indication, all these quality controls, preclinical safety, methods of measuring potency, setting up GMP manufacturing, regulatory work – all that stuff becomes a very different mindset and a huge, huge workstream.
Now, to the big news. You just announced a breakthrough with a ChatGPT-based model that was able to dramatically improve reprogramming efficiency. This is super exciting. Can you tell me more about it?
Yes, it’s been my thesis for quite a long time that biology is too complicated for humans to figure out alone, at least in the larger picture. Obviously, there’s a bunch of low-hanging fruit, especially things that involve single targets or a single pathway where you can disturb one protein-protein interaction and create a helpful effect for a particular disease. But I think there are only so many of those.
Age-related degeneration syndromes are often complex failures that are too hard for people to think about. A human can keep maybe a few different genes in their head at any given time, but then you add the sixth gene interaction with the third and the fifth, and downregulating the second and the fourth, and the network gets too big for humans to keep straight. They’re like, “Ah, can we go back to the single-gene, single-target therapeutics discussion, please?”.
I’ve thought – and hopefully, I get pushback from people smarter than me – that there is an evolutionary bias against single-target diseases. There’s this antagonistic pleiotropy concept where evolution is pretty good at trimming out diseases that pop up earlier in life and interfere with reproduction. Evolution is especially good at making a single mutation and seeing which replicator succeeds the best. It’s harder from a combinatorics perspective for an experiment to be randomly tried by evolution if it requires multiple changes on multiple genes all at the same time. So, I think evolution continually fixes these single-target diseases, and the ones you’re left with at the end of life are this messy, gross soup of multi-gene combinations of things that are starting to fall apart.
I couldn’t agree more on the potential of AI for biology. So, you basically retrained a large language model on all kinds of curated biological data, and the results were amazing.
The models that have been showing lots of traction lately were these LLMs, but they work on sequential data types, like text. A protein sequence is a sequential data type, essentially equivalent to a DNA sequence, but it’s a little closer to actual function, so there’s lower-hanging fruit operating at the protein level. There’s meaning based on proximity in similar ways to text, so how about if we train on that?
The thought was we don’t need to train it entirely from scratch because a lot of the information about proteins is encoded in English. If we co-train a language-based model with a protein sequence-based model, we should be able to capture information that’s in academic papers and annotation databases where humans have put great effort into noting protein functions and relationships. We did some iterations of that and also built a suite of evaluation functions that could give us quicker feedback as to whether the thing we’re training is starting to produce things that look like functional proteins that could actually fold. That was a guide for finding different ways of doing the training.
And your idea of trying of using it to make better reprogramming factors was pretty ingenious.
Well, we’re just already obsessed with those proteins anyway. The model itself was independent and wasn’t specific to transcription factors or Yamanaka factors; we’ve used it for multiple other things. But why not get started on these things? We’ve done a ton of reprogramming and have all kinds of metrics and assays.
Also, they tend to be types of proteins that are a bit hard to interact with using traditional tools because they have large disordered regions, so you can’t come at them from an entirely structured perspective. It just made sense to try these things out and see what happens. We weren’t necessarily expecting that they would be so functional so fast.
But they were. You kind of solved one of the biggest problems in reprogramming: low efficiency.
Yes, it’s so exciting to us that they were so functional. The function was so much better that they’re now in our latest FDA filing for one of the products that we’re taking to the clinic. We ran them through every metric we could think of in terms of whether they make legit, bona fide iPSCs. We wondered, “Is there something horribly, weirdly wrong with them?” It almost seemed too good to be true. So, we ran them through all the quality criteria that people use for iPSCs, and they seem perfect.
I also noticed the model basically made entirely new proteins. You call them enhanced factors, but the model changed 20-30% of the sequence. These could be novel antigens for all we know. On top of that, the model is a “black box,” meaning we don’t know how it did what it did. What are your thoughts on that? Do you see potential problems with safety and immunogenicity?
Actually, in some cases, it’s up to 80%. I think I had already come to terms with the notion that we’re not necessarily going to get to understand how AI does its thing. We’re going to become, at some point, spectators to science as it progresses. So, the fact that we don’t necessarily understand how it did everything – I’m willing to let go of that in exchange for new abilities to do incredibly humane things.
In terms of immunogenicity, it’s definitely a concern. For sure, the safest way is to use these initial proteins on cells outside the body, where they’re not exposed to a systemic immune system. The harder level will be if we want to use these to engineer therapeutic proteins that are circulating in the body. Unless and until we can apply an additional transform to the outer surfaces of the proteins to create a sort of “humanness” criterion – which we’re actively working on – it may be harder to employ them as random therapeutic proteins.
Do you have any thoughts on how we can speed up this process even more, such as with robotic labs for data generation and validation?
I think this is going to naturally happen. People have gotten extremely excited about robotic everything lately, and we’re in the elbow of an exponential curve on robotics. People seeing AI take off is a clear signal that we can build robots now that would not be dumb. In the past, it was demotivating; you could make this great robot, and it would just stand there and not know what to do. But now they’ll know what to do. We’re seeing billions of dollars invested in robotics that will be operated by AI.
In terms of pre-AI robotics, we’re doing a lot here at Retro. We’re supporting an open-source ecosystem called PyLabRobot that allows us to organize different laboratory instruments into clusters that can perform complex workflows for us, faster and more accurately than having humans do it. It’s better to use human brains for inventing the next experiment than having them sit there and tediously execute the last one.
We’ve noticed that ChatGPT is actually pretty good at writing code for PyLabRobot, which is cool. It’s an exciting vision. AI is going to be able to do more of the actions that create more data for the AI to get smarter, producing even more of the actions. We’re excited to be embedded right into one of those feedback loops.
Which brings me to my last question. You started Retro with a goal of extending human healthspan by 10 years. Have your ambitions and your ETA to target changed in the last five years, especially now that you’re using tools like LLMs that we didn’t think we’d have?
I hesitate to predict the future because such predictions are usually wrong. Us having to do clinical trials means we don’t understand biology. We can have an idea and think something is good, but then you must try it out in humans, and at least 80% of clinical trials fail. For me, this means that no one should be taken seriously if they are very confidently predicting the future.
But I could say that if everything goes well, our first drug should be out and prescribable by physicians by roughly the end of the 2020s. There’s a question of how much healthy lifespan extension we can get from making a significant dent in Alzheimer’s, but I think it’s a lot. Because of the regulatory environment we’re in, we have to think about everything in terms of prescribing for specific diseases.
In the meantime, we will operate within the organized constraints of the existing regulatory system, which exists for a purpose and is actually pretty reasonable in lots of ways. At the moment, it doesn’t slow us down hardly at all. The kinds of constraints and processes that are requested by a typical health authority right now don’t seem extreme to me.
I have all of my program leads apply this heuristic they call the “daughter test,” which is that if it were your daughter who had this disease and you’re making the Retro medicine for her, what tests would you want to run? Would you skip the six-month immunogenicity test for this particular therapy and just go straight to injecting it in her veins? Or would you want to run the test? When people roll their eyes about the FDA making us do a test, I’m like, “Okay, first I want to see the list from you of what you think actually matters.” And then I’m going to compare it to the FDA list and – oh, look at that. By and large, they’re pretty much the same.



















 In the heart of San Francisco, a tower in the downtown area is transforming into a center for longevity, artificial intelligence, cryptocurrency, and robotics.
In the heart of San Francisco, a tower in the downtown area is transforming into a center for longevity, artificial intelligence, cryptocurrency, and robotics. Rejuve.AI is a company founded by Jasmine Smith and well known AI researcher Ben Goertzel. Recently, they have launched a new longevity app, and Arkadi caught up with them to find out more.
Rejuve.AI is a company founded by Jasmine Smith and well known AI researcher Ben Goertzel. Recently, they have launched a new longevity app, and Arkadi caught up with them to find out more. The Longevity Summit Dublin has become quite the go-to event in the longevity community. The event first launched in 2022 and has grown in popularity since then.
The Longevity Summit Dublin has become quite the go-to event in the longevity community. The event first launched in 2022 and has grown in popularity since then.