Amyloid-Fibrinogen Complexes Exacerbate Alzheimer’s in Mice
- Synergy is not always beneficial.
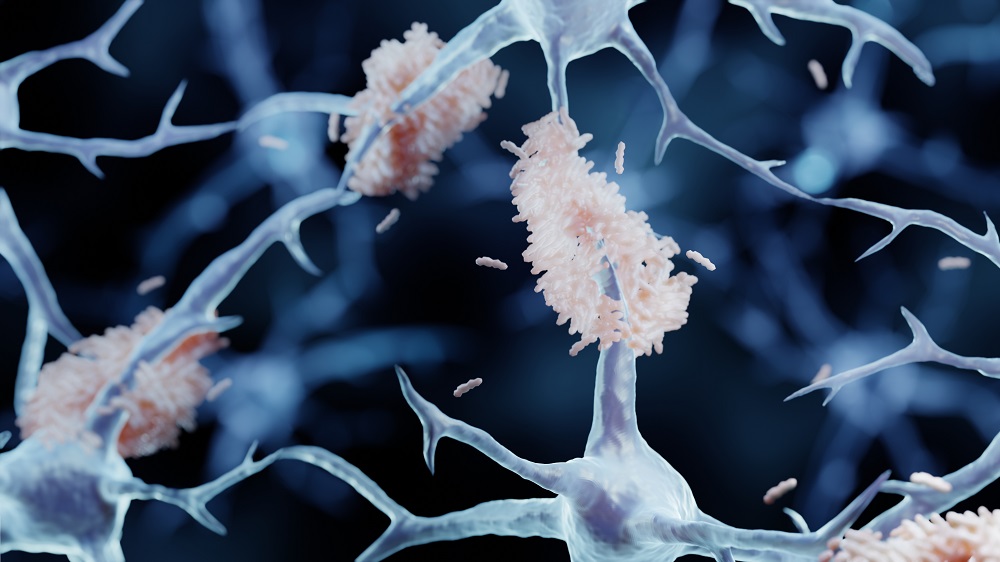
- Amyloid beta or fibrinogen are harmful to neurons in large quantities, but their combination is dangerous to cells in much smaller amounts.
- In mice, this combination led to pathogenic tau accumulation, another hallmark of Alzheimer’s disease.
A study from Rockefeller University suggests that an unholy duo of two proteins causes harm in much lower concentrations than either of them alone. This points to a possible route for intervention [1].
When amyloid met fibrinogen
Amyloid beta (Aβ) and tau proteins are the usual suspects in Alzheimer’s disease. However, focusing on either of them has not been enough to explain all the intricacies of this deadly illness. This group has previously demonstrated that such complexes might be relevant to its progression, and this study expands the search by investigating the complexes that Aβ42, the most damaging type of amyloid peptide, forms with another protein, fibrinogen.
Fibrinogen is the precursor to fibrin, the protein that regulates blood clotting. Normally, fibrinogen should not be present in brain tissue. However, as the blood-brain barrier (BBB) deteriorates, which is one of the hallmarks of Alzheimer’s, fibrinogen seeps through it [2] and interacts with Aβ peptides. The question the researchers asked was, if Aβ and fibrinogen bind to each other, does their partnership actively damage synapses and the BBB?
Wreaking more havoc together
The team started with an ex vivo mouse model: organotypic hippocampal slice cultures (OHCs), which are living 400-µm slices that preserve local circuitry. The researchers treated the slices with Aβ42 and/or fibrinogen in various concentrations, or their pre-assembled complexes, measuring the levels of two proteins indicative of synaptic activity, SYP and PSD-95.
A low dose of Aβ42 (150 nM) by itself or fibrinogen (50 nM) by itself left SYP and PSD-95 levels unchanged, while a high dose of Aβ42 (500 nM) depressed both, as expected. However, when the same low doses (150 nM Aβ42 + 50 nM fibrinogen) were administered as complexes, synaptic proteins plummeted as much as with the high Aβ dose.
“It takes a larger amount of Aβ or fibrinogen alone to cause serious damage in the Alzheimer’s brain,” said Erin Norris, research associate professor in the laboratory of Sidney Strickland at Rockefeller. “But when the two complex together, you only need very small amounts of each to cause damage. There’s a synergistic effect with Aβ and fibrinogen.”
When the researchers pre-incubated Aβ42 with a molecule that blocks the fibrinogen-binding site, the synaptic loss was prevented. This pins the effect on Aβ-fibrinogen binding, not merely on having both molecules present.
The team moved on to in vivo experiments in mice. After an intracerebroventricular (ICV, directly into the brain) infusion, mice that received pre-formed complexes showed reduced hippocampal SYP and PSD-95. Conversely, equal or even higher single-agent doses did not cause this effect. Blocking complex formation erased the synaptic damage signal, just as in slices.
The damage to the brain caused by the Aβ42/fibrinogen complexes went beyond synapses. The researchers also examined phosphorylated tau181 (p-tau181), a widely used early Alzheimer’s biomarker and a biochemical sign that tau is entering a pathogenic state. Just like in the previous experiments, only the complex triggered an increase in hippocampal p-tau181, while neither Aβ42 nor fibrinogen alone did.
Microglial activation occurs when microglia, the brain’s supporting cells, enter a pro-inflammatory state. Two of its markers, CD68 and GFAP, showed a similar picture in that they were boosted by the complex but not by Aβ42 or fibrinogen alone.
A vicious circle?
Finally, the same happened with four key markers of BBB integrity. Consistent with a BBB breach, the endogenous mouse fibrinogen and albumin, two blood proteins that should not be in brain parenchyma, appeared at elevated levels in the hippocampus after complex infusion.
“We wanted to really show the damage – to zoom in on exactly how pre- and post-synaptic terminals were being harmed,” said Research Associate Elisa Nicoloso Simões-Pires. “We showed that the complex actually induces blood-brain barrier leakage, when the proteins alone did not. Disruption of the blood-brain barrier allows for blood proteins to cross into the brain, which leads to additional harm.”
“Only recently, with a number of breakthroughs in the field, did people begin to believe that the vascular system is involved in AD pathogenesis,” said Norris. “Since our initial findings, we’ve been focused on studying the mechanisms that explain how a dysfunctional vascular system impacts AD.”
The researchers also ruled out a different known mechanism of fibrinogen, which binds the protein Mac-1 on microglia to drive harmful activation and dendritic spine loss. In Mac-1 knock-out mice, Aβ42/fibrinogen complexes were just as harmful, suggesting that the effect was Mac-1-independent.
These findings could offer new directions for the study of Alzheimer’s, which has not been particularly successful in the last decades. They also underscore the importance of early intervention when Aβ levels are still low but the cardiovascular damage is already happening. Interstingly, previous work by the same group shows that lecanemab, an approved drug for Alzheimer’s, acts on Aβ/fibrinogen complexes [3], but it is probably not the optimal way to tackle them.
“It’s not a simple disease,” Simões-Pires said. “A lot of other factors can induce neurotoxicity, and we certainly do not propose that inhibiting this complex formation would cure AD. But perhaps targeting this complex would alleviate some of the pathologies and be even more effective in combination with other therapies.”
Literature
[1] Simões‐Pires, E. N., Torrente, D., Singh, P., Strickland, S., & Norris, E. H. (2025). Synergistic effects of the Aβ/fibrinogen complex on synaptotoxicity, neuroinflammation, and blood–brain barrier damage in Alzheimer’s disease models. Alzheimer’s & Dementia, 21(5), e70119.
[2] Sweeney, M. D., Sagare, A. P., & Zlokovic, B. V. (2018). Blood–brain barrier breakdown in Alzheimer disease and other neurodegenerative disorders. Nature Reviews Neurology, 14(3), 133-150.
[3] Singh, P. K., Simões-Pires, E. N., Chen, Z. L., Torrente, D., Calvano, M., Sharma, A., … & Norris, E. H. (2024). Lecanemab blocks the effects of the Aβ/fibrinogen complex on blood clots and synapse toxicity in organotypic culture. Proceedings of the National Academy of Sciences, 121(17), e2314450121.







